It’s been almost two years since my previous post on Tissue and Bone Level implants.
And while I thought this was just a piece of “old news”, it turned out it was everything but an old discussion..! In the 2 years that followed, almost everywhere I’ve been there would be someone who would approach me to talk about this post. Agreements, disagreements, corrections, additions, omissions and everything in-between, I guess it only shows that one of the oldest discussions in Implant Dentistry is still a heated debate. To do justice to this discussion I had to come back with the summary of what I have learned since then, so here we go…
by Nikos Mattheos, DDS, MASc, PhD
It's true, it's not just about Peri-implantitis
My first analysis was focused on the risk of Peri-implantitis, as this was a more tangible goal from a scientific perspective. Nevertheless, I have to admit that there are no “sealed compartments” in implant dentistry. It’s all a comprehensive treatment and complications might manifest clinically in ways different to their actual origins. After all, it was our study which showed that patients with technical complications are 3 times more likely to have biological as well. The comments I received call for a comprehensive view of the differences as well. Trying to see the big picture now and let’s start from the easy parts…
Tissue level, bone level and marginal bone loss
Two years ago I wrote that I find no reason as to why Tissue level implants would be any better in relation to marginal bone loss or tissue inflammation when compared with bone level. Has anything happened since then to change my mind?
No. And Yes. (sorry I cannot find a more specific way to say it!). To be clear, the evidence I have seen in the last couple of years has only strengthened my confidence about the importance of a narrow angle emergence for the stability of the peri-implant bone.
In particular what we call the “Deep” angle, is a critical determinant of the early marginal bone loss or “remodelling”. This is not the approximate “emergence angle” as drawn on the contour of periapical radiographs, but the angle at the bottom of the implant abutment, exactly where it ascends from the bone level. Place an abutment with Deep angle close to 45o and you will end up losing much more marginal bone due to remodelling, than with a narrow 15o abutment (Souza 2018). If the deep angle is so important to maintain marginal bone loss, do the Tissue Level implants have any advantage to that end?
Not by default, but there could be an indirect advantage. If we accept that the deep angle matters, Tissue Level implants do exactly this: they “lock” the deep angle within a certain array of options. This will limit our ability to individualise the design, but at the same time it will prevent anyone from overcontouring straight from the level of bone. Looking at the geometry of the Tissue Level implants, one can see directly that they do not have just one angle in the collar. Instead, there can be different angles from 2o to 28o depending on the implant type and dimensions. The good news however is that it never goes beyond 30o. In particular the good old original Standard Tissue Level would ensure at all times a height of 2.8 mm with a fixed deep angle of only 13o ! You can see it as a built-in, fool-proof protection mechanism against bad design: no matter how you try, you just can’t mess it. The collar of the implant will always “lock” the first 3 mm of your supracrestal complex into a biologically acceptable configuration. Interestingly, the new TLX collar design extends this to also a convex profile, which might add more to the benefit of the collar. I do not know of the actual angles of the TLX, but they appear similar to me.
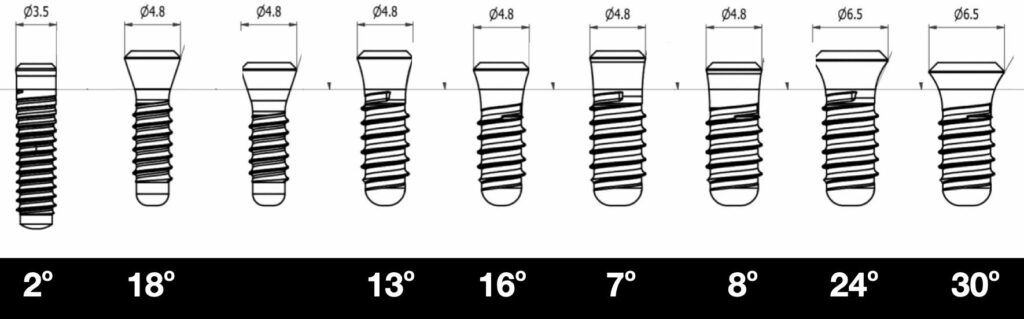
Tissue level implants are not the same in terms of deep angle, even within the same brand (Straumann S, SP in the picture above). Depending on diametre and height of collar, angle changes but is never wider than 30o.
Paradoxically, the very element that limits the expert designer from creating a purpose made emergence profile is the same that prevents a bad designer from creating an unacceptable one.
Paradoxically, the very element that limits the expert designer from creating a customised profile is the same that prevents an ill-trained designer from creating an unacceptable one. This might have been a very important element of the success of the Tissue Level implant in the early days, when we were unaware of the supractestal complex design implications and it might be still very important for novice users. Of course, the solution is not the choice of implant, but to make sure that everyone who offers implant service is well trained and aware of the implications of prosthetic design.
In conclusion, I still maintain the view that a Bone Level implant is a versatile and effective platform, which allows more freedom for individualisation than the Tissue level. That is of course in the hands of a well-trained clinician, who understand the basic design principles of the Implant Supracrestal Complex. On the other hand, if in the hands of an ill trained clinician, a Tissue Level will act as the safety break: it will prevent the worse of the design mistakes. That might be a significant advantage in large scale, which however would go unnoticed in the studies, as most of them are conducted at University clinics by experts who are well aware of design principles and maintenance. At the same time, having been a recipient centre for all sorts of complications in the last decade, I have seen many impossible prosthetic designs on Tissue Level implants, which would probably never make it far if they were on Bone Level implants.
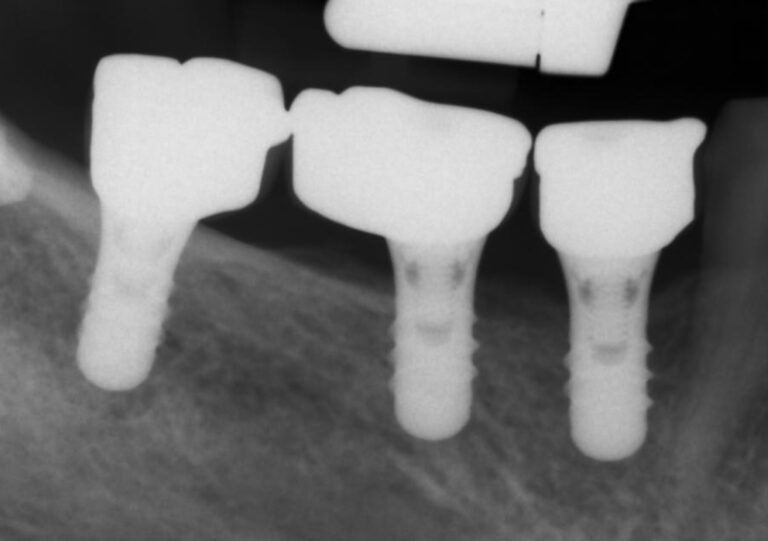
Prosthetic designs such as the implants above would go against anything we know about proper emergence profile. On bone level implants, such a prosthesis would have caused massive marginal bone loss. The collar however, forcing 2.8 mm of height under 13o appears to have saved the day.
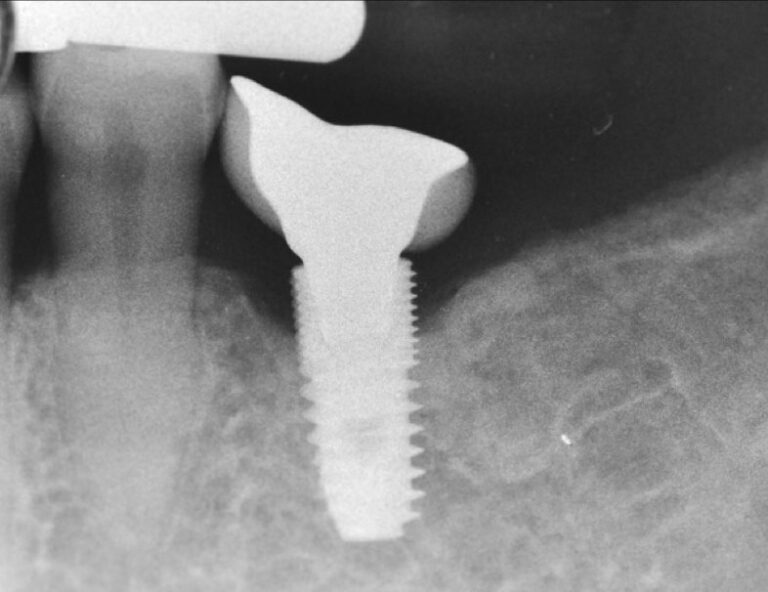
A similar problematic prosthesis design as before, only here directly on the bone level platform. No surprise that we run out of luck with this design and we can’t blame the bone level implant for the marginal bone loss…
the 2.8 mm Tissue Level collar acts as a built-in fool-proof protection mechanism against bad design: even if you don't know how to design it, you just can’t mess it too bad
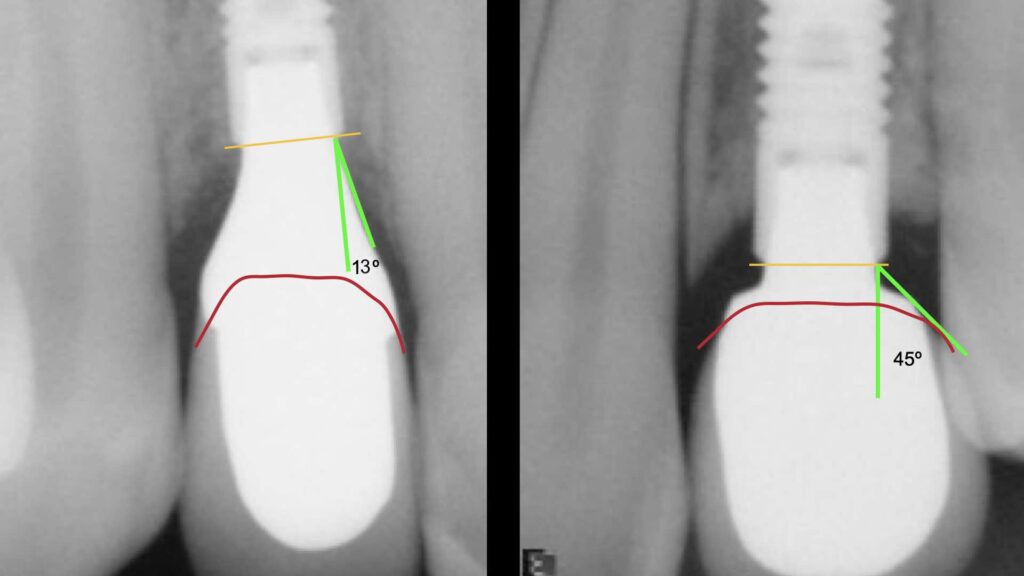
As much as the optimal individual design at the left would be not possible with a Tissue Level implant, also the unfavourable design to the right would have not been allowed on a Tissue Level implant!
Any news with Peri-implantitis?
maybe disappointingly so, but I would not have much to add to the last post with regards to actual risk for peri-implantitis. No new study or discussion has surfaced that would point to any difference to the risk for peri-implantitis when Tissue Level or Bone Level implants are used. Some authors have started suggesting that early marginal bone loss or remodelling can actually predispose or increase the risk for to peri-implantitis. This is however based on retrospective radiographic studies, which use the very radiographic criterion of marginal bone loss to define peri-implantitis. using as predictor of the disease thevery measurement you use to define the disease can seriously mess conclusions in cross sectional or retrospective studies. In one of our clinical studies we have seen that early marginal bone loss correlates with marginal bone loss at at later points, even at the absence of peri-implantitis. That is as simple as the fact that those who lose a lot of bone at the first six months are the same who show up having lost most bone at 5 years, even if the rate of bone loss significantly slows after the initial loss. Peri-implantitis, as an inflammatory disease, does not start with marginal bone loss, but with plaque induced inflammation at the mucosal margin of the prosthesis. How the early marginal bone loss can interfere with this process is for me far from clear at this point. This might be a good topic for a more detailed discussion in the future. For now, I see no reason to change my view that there is no difference in the risk for peri-implantitis from using tissue or bone level implants.
What about technical complications?
Technical complications is a whole new area that we have not discussed previously and it could certainly be part of decision making. None the least, as it has been shown that increase of technical complications can be linked to more biological complications as well. Could it be that Tissue Level implants suffer from less complications than Bone Level? Again, to answer that, one would have to define what we are comparing. Trying to compare technical complications between Tissue Level and Bone Level implants of the same brand for example would be an interesting but very challenging research exercise and I have not come across of any clinical studies that have actually shown a significant difference. Nevertheless, looking indirectly at some mechanics, in-vitro and non-comparative studies, one could reasonably expect different behaviour between the two implant configurations at certain conditions.
Studying the Synocta connection of the Straumann Tissue Level implant, one can easily see how solid and stable this configuration is. There is an element of this connection that is impossible to imitate at bone level implants and this is the “double squeeze” of the abutment between the oblique head of the abutment screw and the external part of the prosthesis that rests on the oblique implant shoulder. As we tighten the screw, the oblique head presses the abutment outwards against the implant wall. At the same time, the part of the abutment resting on the oblique implant shoulder presses the implant wall inwards, just like the ring of a barrel. The stability of this configuration to lateral forces is unparalleled by any platform switching connection, where inevitably the abutment can only be wedged internally and press outwards. At the same time, the 2.8 mm high collar of the tissue level implant will bring the fulcrum of any lateral forces much more coronally than in Bone Level implants reducing the damaging effect on the connection.
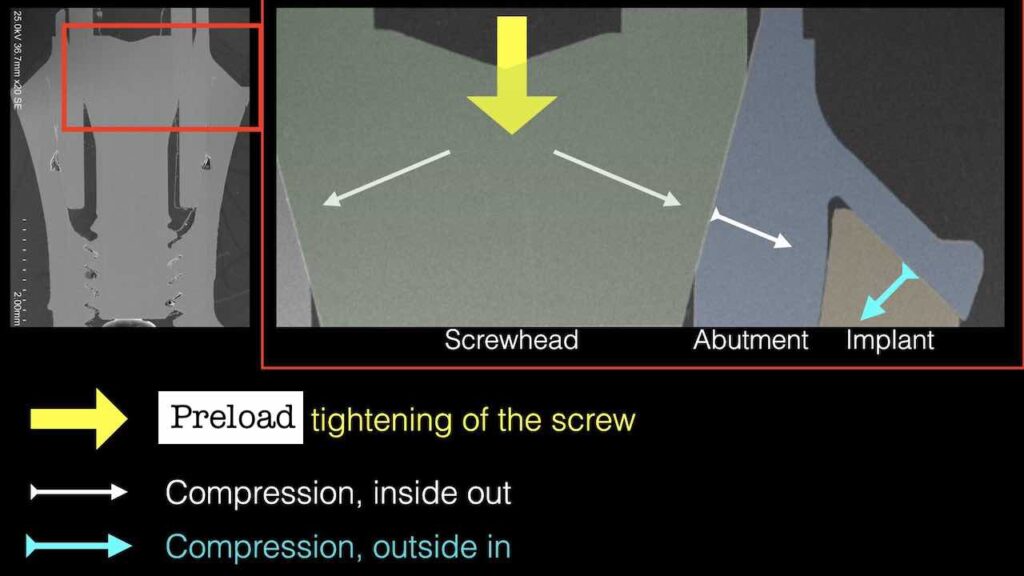
The “double squeeze” of the Synocta connection at the Tissue Level implant as seen under the Scanning Electron Microscope (Mattheos, Larsson, Janda et al 2017). Note how the abutment shoulder is compressing the connection inwards, adding stability on the oblique implant shoulder.
Would all this matter clinically? Possibly in some extreme cases such as for example when supporting an occlusally loaded cantilever, according to my friend Professor Stephen Sadowsky from the University of the Pacific in USA . He made a convincing case of Tissue Level implant being a much safer platform to support cantilevers, based on a 10 year retrospective study, (which however was not comparative) and a computational one. Would this influence also non-cantilever or mainstream cases? That is yet to be seen, as clinical studies I am aware of have not reported such a difference. The capacity of the Bone level connection is well within the requirements of most clinical scenaria. It is reasonable to assume however that the margin of “technical” tolerance of the Tissue Level implant connection would be higher than the equivalent in a Bone level platform. And is only common sense that screw loosening at Bone Level could be more damaging than at Tissue Level.
Conclusions, Vol 2 !
As what I initially thought as an “academic discussion” kept being vividly debated, I do not see any dramatic shifts in any direction. It is well obvious to me now that Tissue Level implant design was well ahead of its time, and today we understand more why. It will not prevent peri-implantitis, certainly not any more than any other implant. But it could prevent novice and unaware clinicians from some of the most common restorative mistakes.
Today we understand a way lot more about the complex interactions of biology and technology, tissue and components. The Bone Level is a versatile platform which allows for much more flexibility to address the individual anatomy with safety and predictability, thus it has taken a primary role in implant therapy worldwide. I would still use the Tissue Level, but with a more narrow scope of indication. Even then, my decision would not be based on expecting to prevent peri-implantitis, but rather on how much the emergence profile I aim to create matches the one the Tissue Level implant allows for.
At the end of the day, both platforms will work fine, as long as you select the proper case and you know what you are doing when designing the Implant Supracrestal Complex
Hear the latest news first: Subscribe to my newsletter!
References
1. Becker CM. Cantilever fixed prostheses utilizing dental implants: a 10-year retrospective analysis. Quintessence Int. 2004 Jun;35(6):437-41. PMID: 15202588.
2. Mosavar A, Nili M, Hashemi SR, Kadkhodaei M. A Comparative Analysis on Two Types of Oral Implants, Bone-Level and Tissue-Level, with Different Cantilever Lengths of Fixed Prosthesis. J Prosthodont. 2017 Jun;26(4):289-295. doi: 10.1111/jopr.12388. Epub 2015 Dec 14. PMID: 26662575.
3. Bilhan H, Erdogan O, Geçkili O, Bilgin T. Comparison of Marginal Bone Levels Around Tissue-Level Implants with Platform-Matched and Bone-Level Implants with Platform-Switching Connections: 1-Year Results of a Prospective Cohort Study with a Split-Mouth Design. Int J Oral Maxillofac Implants. 2021 Sep-Oct;36(5):945-951. doi: 10.11607/jomi.8891. PMID: 34698721.
4. Acharya A, Leung MCT, Ng KT, Fan MHM, Fokas G, Mattheos N. Peri-implant marginal bone loss rate pre- and post-loading: An exploratory analysis of associated factors. Clin Oral Implants Res. 2019 May;30(5):410-419. doi: 10.1111/clr.13424. Epub 2019 Apr 16. PMID: 30921476.
4 thoughts on “Tissue Level versus Bone Level implants: Vol. 2 !”
great read and very detailed analysis, thank you! So do you see any advantages for tissue level any longer in a practice or you believe you just can use bone level for everything? It seems that many people still prefer tissue level and companies release new versions.
I think the tissue level implant has been a great implant and I still use it a lot for single crowns and small span bridges.
I have been using both tissue level and bone level implants for many years with inseparably good results. Surprisingly, I recently had a patient who requested a tissue level implant from me. No idea how he got the information or what was it that influenced his preference, usually I do not discuss the choice of the implant design with the patient, mainly because it never occurred to me that they would be interested or understand the differences. This made me reflect. Do you discuss the selection of implants with your patients, or even offer them a choice when it comes to bone or tissue level?
Again thank you for your great page, so much insight in the details of implant dentistry!
Dear Ealin, very interesting experience, thank you for sharing here! I actually haven’t had any patient so far requesting in particular Tissue Level implants, although I do have from time to time patients asking for a specific brand or wanting to know more of brand choices. I would usually discuss the brand with patients, as it has quality and cost implications, so I always tell them in the quote which implant system we will use and the original components. I think this is an important part that the patient has to be aware and share the decision. However, when it comes to choice between Tissue Level or Bone level, I have never really discussed this with patients. I doubt that the average patient will be in position to comprehend the differences and even more to share the responsibility of such a decision. If they think they know it might be typically because they have fallen for some marketing claims (or they have read my blogposts maybe:), so maybe some supereficial “knowledge” might be what drives them to request a specific type. So if a patient comes up with such a request, I think I will be happy to discuss with him, at the basis of his understanding, but I will not start such a discussion at my own initiative… patients today come having googled everything, which is a blessing and a curse at the same time! Thank you for bringing this up!