Whether we need keratinised Mucosa around implants or not, is a discussion that echos the decades-long debate of attached gingiva around teeth. In this article we reflect on the need -or no need- and then we discuss the technicalities of an augmentation technique which combines the benefits of free gingival and connective tissue graft which might be of help in implant cases!
To keratinise or to not keratinise?
Lack of keratinised mucosa can be often a cause of concern around dental implants. Whether keratinised mucosa is essential and how much has been the subject of a long debate in implant dentistry, which in essence reminded me of the similar debate about the presence Attached Gingiva and Gingivitis. Back then, a series of animal experiments by Lindhe and his team had concluded that a zone of attached gingiva was not essential to prevent gingivitis in the presence of oral hygiene (1,2). As a result, interventions to increase the width of attached gingiva around teeth were rarely seen or promoted, especially as preventive. With the spread of implants however, this debate was “reheated” and served again with a slight different twist. Surgical techniques for the development or increase of keratinised Mucosa around implants have been increasingly developed and applied. Should there be a difference when it comes to implants? I am not sure. But the truth is that peri-implant tissue is different in many aspects, as it is a structurally compromised tissue when compared with the periodontal.
Looking at the literature, there is a large number of papers which shows no difference with regards to bleeding on probing or plaque indices in the absence of keratinised Mucosa, but then again there is a smaller but substantial number of papers which show a difference. And when a difference is shown, it always favours the presence of keratinised mucosa. Maybe that was the reason for the very “diplomatic” statement of the 2017 World Consensus Workshop in Periodontology which reads:
"The evidence is equivocal regarding the effect of keratinized mucosa on the long-term health of the peri-implant tissue.It appears, however, that keratinized mucosa may have advantages regarding patient comfort and ease of plaque removal."
2017 World Workshop on Periodontal and Peri-implant Diseases
Needs, desires and simply letting go..!
It is clear to me that even if not essential, keratinised mucosa is certainly desired around implants. Buddhism would teach you how to separate your needs from your desires and how to let go of the latter, but our problem here is of less academic and more practical nature! In daily practice, the tricky question I face is not if keratinised mucosa is essential, but how far am I willing to go in order to secure it in the cases that I don’t see it. Is a surgical intervention justified at all times when we lack keratised mucosa? When is it worth the trouble, when not and when is too risky? And here there is not much certainty to guide us. Whether to intervene surgically to correct or improve mucogingival conditions is not an easy decision and one needs to carefully assess the conditions, as often surgery has the risk of deteriorating the problem. It is reasonable to anticipate that it will be beneficial in some cases, while in other it might be not indicated or even too risky. At the end of the day, it is a judgement call, that we all have to take after ensuring we have taken in consideration all local anatomic, prosthetic as well patient-based parametres. Ideally, prevent the problem by ensuring that you preserve or “engineer” a narrow zone of keratinised tissue during the implant placement surgery.
If you encounter an implant with no keratinised mucosa around it, the problem sometimes appears as aesthetic, in other cases it might predispose to long term problems and inflammation. One of the most critical determinants is your diagnosis: study carefully the Implant Supracrestal Complex every single time. Problems that manifest as mucogingival such as lack of keratinised Mucosa, might in reality be caused by underlying predispositions such as malposition of the implant or improper prosthetic design. In cases like these, intervention on the soft tissue without modifying the underlying problems might simply fail to solve the problem or even make things worse. Read more in our past article on hidden predispositions of implant complications and how to conduct the proper detective work.
Established Mucositis and swelling buccal of the 22, initially attributed to absence of keratinised mucosa and thus referred for soft tissue augmentation. Studying the CBCT however, in combination with the clinical examination, one can see the main problem here to be the implant position. In particular the bucco-palatal angle results in the implant shoulder being too buccal. As a result the cement retained prosthesis is also protruding in its apical part, resulting to recession beyond the mucogingival line. Unless we can correct the implant position and the crown, any intervention targeting the soft tissues alone is likely to make the problem even worse.
What do I do?
Hmmm, I do not have a simple response, as I will decide on a case-by-case basis. In general, I will not routinely intervene surgically for the increase of the keratinised mucosa and in many cases where the oral hygiene appears effective I would simply follow up with strict maintainance. There might be certain exceptions though, such as for example the case of mandibular locator overdentures. As the bone resorption pattern of the mandible brings the mucogingival margin very much to the lingual side, implants placed for locator abutments in the anterior mandible are often left outside the keratinised zone. I have seen very often problems of inflammation around implants supporting overdentures when there is no keratinised mucosa around the locator abutments. This could happen for a variety or reasons that can be both anatomic, patient-based and also due to the removable nature of the overdenture. Whatever the case, I am more inclined to intervene even preventively for soft tissue augmentation in overdenture patients.
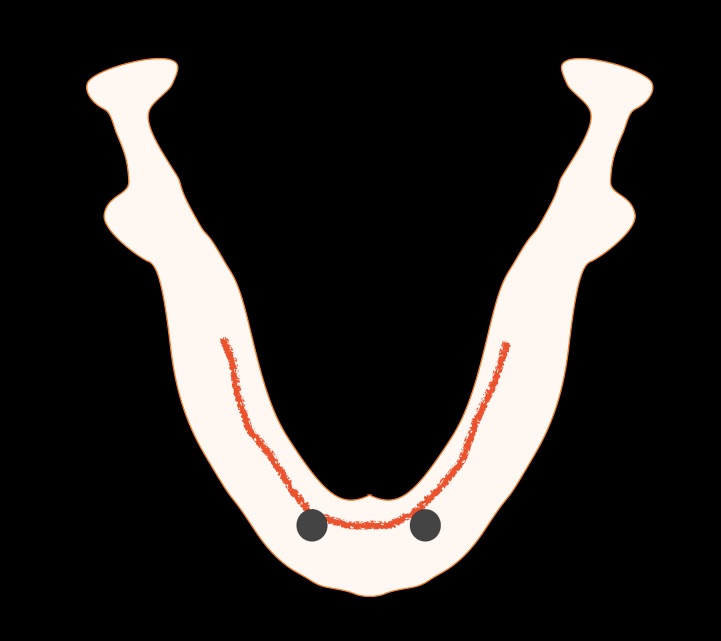
The bone resorption pattern in the edentulous mandible often results in the mucogingival line to be transposed rather lingual. This means that the bulk of the volume of the mandibular bone is under the mobile oral mucosa, rather than the keratinised. Due to possibly the local anatomic characteristics but also the removable nature of the overdenture, lack of keratinised mucosa in such cases can increase the risk for inflammation and difficult to resolve problems of the soft tissues. In such cases I would recommend preventive increase of the keratinised mucosa width in the position where the implants will be placed


Locator abutments of mandibular overdenture, burried under the swollen and inflamed oral mucosa. Resolution of the inflammation in such cases is very challenging, but unless some surgical adjustment of the peri-implant tissues takes place the problem can be recurrent.
Baloon-style swelling of the tissues around locator abutment of mandibular overdenture, combined with Peri-implantitis. Adjustment of the soft tissues in combination with teh peri-implantitis surgery is essential in such cases to minimise the risk of recurrence.
The hybrid CT-Epithelial graft
If you are confident the problem diagnosed is limited in the soft tissue and an increase of the keratinised zone is indicated, the good news is that you don’t need much tissue. A minimally invasive approach to develop a couple of millimetres of keratinised mucosa will be more than enough. A recent review by Lin et al (3) found that surgery in the absence of keratinised zone was effective to increase it to about 2-3 mm. However, surgery to increase an existing keratinised zone of 2mm , had very little additional value. Consequently, having a couple of mm of keratinised zone is good enough. If you have it, be happy. If you don’t, design an intervention that is minimally invasive and will target the development of this couple of millimetres with the least risk and hassle.
In such cases, a the Hybrid CT-Epithelial graft is one of my preferred methods of action, as it is minimally invasive, ensures better healing conditions and can achieve both keratinisation and volume augmentation. For me this has been more of a “common sense” approach rather than a whole new technique, so I never bothered much with the name or the description. Nevertheless, as many colleagues and students have asked me frequently about it, I had to put my head down to try to describe it a bit more systematically, and thus help also myself to better understand what I was doing…indeed, you learn twice when you try to teach 🙂
As the actual technique might be difficult to fully comprehend by watching only clinical videos, I have prepared a quick “explainer” video where you can see the full design and rationale of this technique.
Rather than a whole new technique, I have always seen this graft as a “common sense” approach, which however has some important design parametres to follow and some biological fundamental principles. Let me explain more details about the design and rationale in this short schematic “explainer” video.
PS: apologies for the Ambulance passing at 3:40! It is not a sound effect, I just have my office in the hospital 🙂
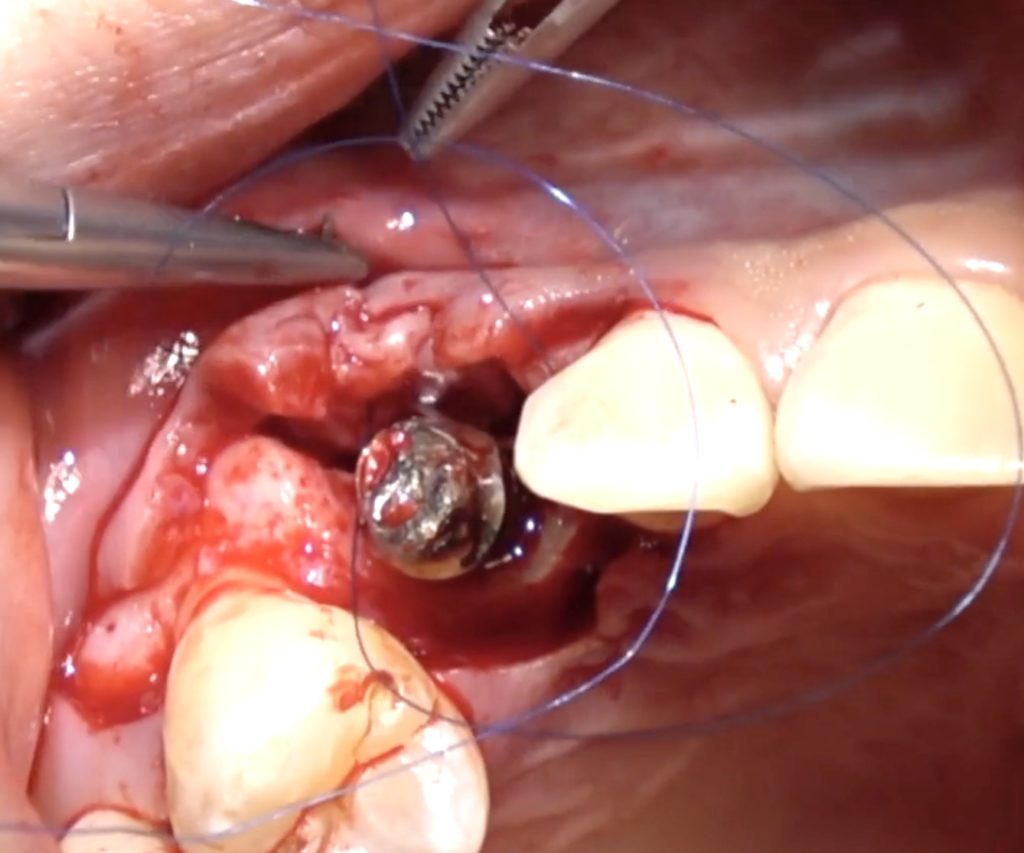
Here is a clinical video of a procedure where the CT-Epithelial graft is applied to create a 2-3 mm zone of keratinised mucosa buccal of an implant crown in the mandible. The graft is harvested from the palate and applied with the procedure explained before
What about Peri-implantitis
Connective tissue grafts have been also proposed as part pf peri-implantitis surgeries and I think in certain cases they certainly have a purpose to fulfill. I have used the Hybrid CT-Epithelial graft often in peri-implantitis surgery, especially in cases with absence of keratinised mucosa and very thin peri-implant tissue. You can watch such a surgical case in our online Masterclass on the management of implant complications to the right!
Learn the latest news first, subscribe to my newsletter!
Do you want to get deeper into complications and how to manage them?
A Online Masterclass in Implant Complications might be something for you!
Start today with the free Module 1 and join a vibrant community of learners!
All you need to know about preventing and managing the most common problems of implant therapy, from biological to technical and all in-between!
www.masterclassindentistry.com
References
1. J Wennström, J Lindhe. Role of attached gingiva for maintenance of periodontal health. Healing following excisional and grafting procedures in dogs J Clin Periodontol 1983 Mar;10(2):206-21.
2. Wennström J, Lindhe J, Nyman S.The role of keratinized gingiva in plaque-associated gingivitis in dogs. J Clin Periodontol. 1982 Jan;9(1):75-85.D.
4. Cho-Ying Lin et al. Impact of timing on soft tissue augmentation during implant treatment: A systematic review and meta-analysis. Clin Oral Implants Res 2018 May;29(5):508-521. doi: 10.1111/clr.13148. Epub 2018 Mar 30.