Back in the army we had an old ambulance which we called “Florence Nightingale”, in an obvious reference to its years in service. We used it to deliver medication and supplies to remote locations of the camp and the driver kept always a small hammer by the windshield.
One day Florence simply refused to start. The driver took the hammer, stepped out, opened the bonnet and hammered the starter 3 times, almost in a ceremonial manner. When he tried again the ignition, Florence started almost immediately to the loud applaud of all bystanders.
Nobody knew where this magic came from. The driver said he had learned the trick from the previous driver. Some said that the legendary hammer came actually with the car from the factory for that very purpose…
Twenty years down the road, while working on a presentation about implant complications, this old story, somehow stroke me similar to how we often perceive implant treatment today… Now what does my old dear Florence have to do with dental implant complications? Well, let me explain more …
Everything breaks down. Machine parts, human parts, relationships, for everything there comes a time when things start to fall apart. Some things we chose to repair, other we let go. It’s a fact we get to accept rather early in life. But then what is it that we call a “complication”? What determines your reaction next time your car refuses to start? Would you curse and swear in disappointment or stoically look for the magic hammer you keep by the windshield?
Usually we would call “complication” any unexpected damage or problem, which requires repair or resolution in order to return to the original optimal condition. But then again, what we perceive as “failure” or “complication” is very much determined by our perception of three key factors:
1) Life expectancy:
We deeply know that nothing lasts for ever. If your 2-year old BMW suddenly refuses to start, you will probably be very right to be pissed off. But if you are driving “Florens” who has already exceeded two life cycles, would you as easily call the starter problem a “failure” or a “complication”?
2) Conditions of use:
This simply implies that there is a right use and an “unauthorised”, “off-label” or “unwarranted” use for every machine. Your new Ferrari might be an engineering marvel, but if you drive it off-road it will soon break down. Will you be then right to call it a complication?
3) Need of maintenance:
This simply implies that Homeostasis needs some active help in its eternal battle against Entropy. Whether it’s our car or our home, we all accept that regular preemptive interventions are required in order to keep things in service. So will we still call it a complication when the car refuses to start if last time the spark plugs were changed was two years ago?


…but what about implants?
Well, here is where things start to get complicated…! Dental implants – mechanical parts implanted in biological tissues – do not differ to any other man made construction: they serve and they break down.
We typically classify as “complications” the sum of the very diverse things that can go wrong in an implant patient, from inflammation (peri-implantitis) to hardware problems such as screw loosening, fractures or porcelain chipping. Then we pack it all into one number reflecting prevalence of events in a period of 5 or 10 years and we discuss in shock how implant treatment is plagued by complications in the medium to long term. But is this the full picture? I’m afraid not. The picture we have today of implant complications is distorted by our absolute inability to define and report complications within the framework of the three key parametres: life expectancy, conditions of use and needs of maintenance.
During a retrospective study in Australia some years ago (1) we learned two interesting facts about implant complications: – First, complications appear to cluster around certain patients.
Lesson Nr. 1: complications are neither randomly nor democratically distributed among the patients. Few guys will get most of the trouble.
Lesson Nr. 2: what we diagnose as “complication” might often be the result of a hidden (and often iatrogenic) predisposition…!
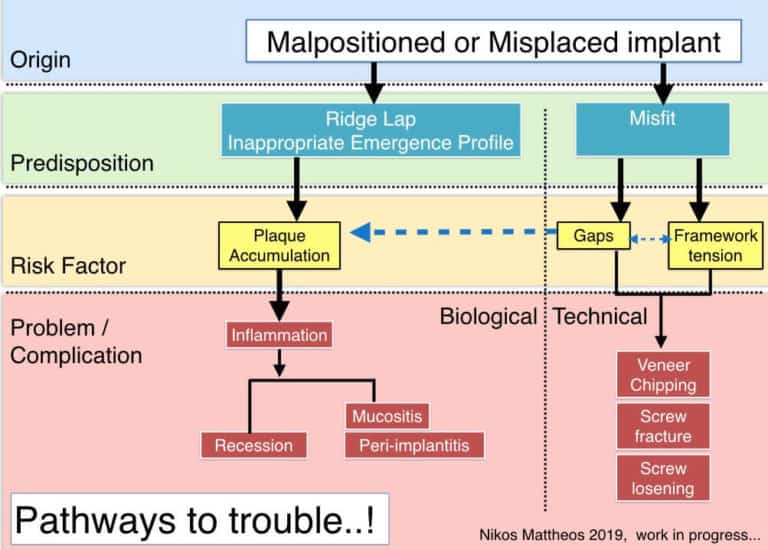
…and here some work in progress!
The idea is to map in a flowchart some of the most common “origins” predisposing to problems by exposing implant treatment to known biological or technical risks, finally resulting in complications. Any suggestions more than welcome!
So, what now?
Well, we got quite some work to do! I’m afraid that a using a “blanket” definition of any possible problem encountered as “failure” or “complication” and collectively reporting diverse events and conditions is only masking the true situation. It also strikes me that the way we approach complications with implants is much different to other rehabilitation treatments. We usually say that maintenance is what you do before things break down and what you do after they break is management of complications. But even this is not clear when it comes to implants. I recall a very vivid discussion we had with our research team during a recent study (2), when we could not agree how frequently an implant overdenture needs relining as part of expected maintenance and when the increased need of relining should be seen as “complication”. So we need to define our game more clearly, but I’m afraid this will be very difficult to do, unless we start defining, reporting and understanding complications under the light of the three key parametres…
1. Life expectancy
Fatigue of hard working metal parts is a reality since the Iron Age, which however the world of implants surprisingly overlooked. We accept that almost every functioning part of our car engine will be gradually replaced as the kilometer count increases. And although we would preemptively replace the clutch plate after 60,000 km, how long can a prosthetic screw last under an implant supported bridge? Would it make sense to replace it pre-emptively at some point? In reality, I (we) don’t have a clue. The way the data is reported on 5 and sometimes 10 year summative numbers, it is very difficult to see in detail how time in function affects mechanical problems .
Peri-implantitis on the other hand is a different game: it is a disease, not a result of fatigue or time in function. As such, it is not inevitable. Peri-implantitis is a complication of implant therapy no more than Periodontitis is a complication of having teeth! But we don’t call periodontitis a complication, right?
2. Conditions of use
This is in my mind the most important and underestimated parameter of the three. Complications will greatly depend on how we choose to use the implants. So what are the necessary conditions of use for implants? You place an implant in the bone, it osseointegrates, you make a crown, patient goes. Is this all?
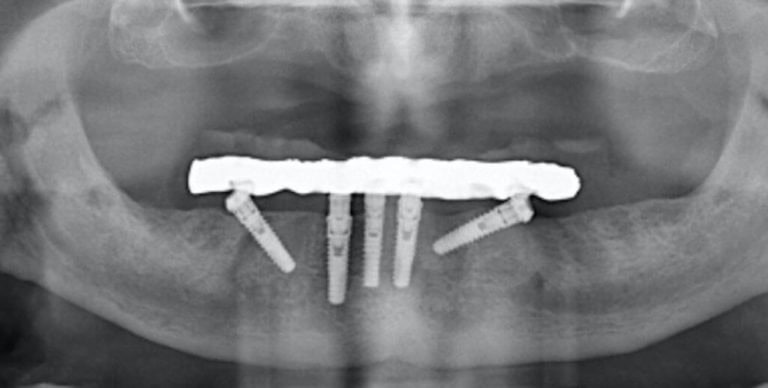
But what if you place an implant in a patient with periodontitis? Or a patient with deficient practice / understanding of oral hygiene? What if you place an implant in unfavorable prosthetic position resulting in an uncleanable prosthesis? In all the cases above, the implant is “predisposed” to trouble. In the terminology of medical devices this would make the implant used “off-label”. Problems will surface sooner or later and then we will pack it together in a summative number as complications. But how many of the implants reported in the literature with complications could actually have been “off-label”? For example, how many studies reporting prevalence of peri-implantitis also report how many of the prostheses were uncleanable? As of today, I know only one (3). This fact might partly explain the wide range of prevalence found in different studies and environments. Complications will occur even when all conditions of use are met, but if we add on top the problems of implants that are predisposed, do we get a fair picture of the problem? Predisposing factors can also be technical. In a series of recent studies (4,5) we found that even a small vertical misfit of 100μm has the potential to increase the risk of veneer chipping by multifold in small-medium span implant prostheses.
3. Need of maintenance
Here we still have some work to do. As of today, maintenance protocols mainly focus on the peri-implant tissues, in most cases directly extrapolated from periodontal maintenance protocols, but there is a large gap in our understanding on how to maintain comprehensively, which includes the technical parts. How to examine the integrity of the prosthesis and all components? When to replace parts? How to identify “predispositions”? How to modify our maintenance protocols when we have compromised and predisposed situations? Now this is a great discussion, but it would take much more than this short article aspires to be…
Conclusively…
It is true, Implant complications are today a very hot topic. Nevertheless, I feel we are far from being able to articulate and quantify the actual problems of implant therapy. The data we have, in the way they are reported do not help to draw the full picture. Complications of implant therapy is a true problem, but it is not always due to an inherent limitation of Implants or an inevitable “tsunami”. Very often when problems occur, there is a “predisposition” in the system, often due to known or unintended compromised decisions, designs or plans from our side. In the end, the only way to reduce complications remains the profound understanding of the biological and technical principles of Implant therapy, so the key is again, proper education.
to Florans, endless source of inspiration and most comfortable ambulance bed during “Parmenion” drills. May you rest in Ambulance heaven
learn the latest news first, subscribe to my newsletter!
Do you want to master implant complications?
Mastering Implant Complications is an practice oriented fully online course, aiming to help busy clinicians, understand, prevent and manage biological and technical complications with implant therapy!
Dr. Mattheos and Dr. Janda, world-class experts with both clinical and research experience in the field, will guide you in an interactive learning experience targeted to improve your skills and help you deal with problems in your practive!
References
- Kim et al.The impact of cantilevers on biological and technical success outcomes of implant-supported fixed partial dentures. A retrospective cohort study. Clin Oral Implants Res. 2014 (2):175-84.
- Zhang et al. Patient-reported outcome measures (PROMs) and maintenance events in 2-implant-supported mandibular overdenture patients: A 5-year prospective study. Clin Oral Implants Res. 2019 (3):261-276.
- Serino, Ström. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009 (2):169-74.
- Löfgren N et al. Influence of misfit on the occurrence of veneering porcelain fractures (chipping) in implant-supported metal-ceramic fixed dental prostheses: an in vitro pilot trial. Clin Oral Implants Res. 2017 (11):1381-1387.
- Janda M et al. Influence of misfit on the occurrence of veneering porcelain fractures (chipping) in implant-supported metal-ceramic fixed dental prostheses. Part II: a Finite Element Analysis study. Int Jour Pros, in press.

5 thoughts on “…it’s complicated! Reflecting on implant complications!”
Hi Nikos! As a prosthodontist from a clinical standpoint as well as lecturer, my view is identical. The primary cause of many problems with implant cases is misplacement of the implant ( eg wrong treatment planning). Lecturing extensively I focus a lot on secondary problems caused by this, so I would gladly participate in any efforts mapping this out. Martin Janda I know from my school days of course and would be happy to combine lecturing with you all !
Regards,
Dear Marcus,
thank you very much for your kind interest and feedback! I wish you a great start in the new year and I hope there will be opportunities to meet and work together in the near future! Stay in touch!
best regards
Nikos
Very interesting articles. Thank you for sharing.
Thank you Ben!
best regards
N
Great content! Super high-quality! Keep it up! 🙂