Part I: Navigating a rapidly transforming environment
by Nikos Mattheos, DDS, MASc, PhD
James Chow, BDS, MDS, OMFS Specialist, FRCDS(Eng), FRCDS(can)
Implants placed in fresh extraction sockets were first documented more than 25 years ago, so one might wonder why “immediacy” took so long time to mature into the mainstream implantology. The progress of a scientific protocol however, is rarely a straight line to implementation. Perceived breakthroughs are often followed by backlash and enthusiasm can be at times interchangeable with periods of caution. In the end, technology is also a major catalyst to help a vision make it safe to the mainstream practice.
How did immediacy develop from the first “immediate” implants into the current modern concept as a workflow? Let’s take a closer look into a long and winding road!
An old innovation..!
If you think that immediate implants are a cool new development, better think twice: it was a hot research topic already in the 90’s and scarily enough, this is already 30 years ago..! Back in 1996, NP Lang the founding editor of Clin Oral Imp Res after an exhaustively detailed study was concluding that “immediate implants are feasible treatment modality with high predictability”, while also documenting less bleeding on probing around immediate than conventionally placed implants. Back then he was placing the “ITI implants” in fresh extraction sockets with or without guided bone regeneration and transmucosal healing. Well ahead of its time you might think. Interestingly, by the time I joined his department in 2005 he was rather critical of immediate implants, and so would also remember him most of our Hong Kong colleagues and students. To think of what could have possibly happened, let’s get back to 1996 and follow the steps of an exciting journey.
Although publications about immediate implants were appearing all through the 90’s, long term evaluations start to show towards the end of the decade. In 1997, Schwarz-Arad and Chausu published 4-7 years follow up of 95 immediate implants placed with submerged healing and showed a very good survival rate of 94.7 %. Just a year later, in 1998 the same authors growing obviously encouraged by the documented success, they take the method one step further and publish 9 cases where the implants were placed flapless in the extraction sockets, augmented with autogenous chips and left to heal transmucosally with only some retaining sutures. And guess what, it all worked well.
By the time I start my own journey in Implant Dentistry around the turn of the millennium, the euphoria on immediates continues and Brånemark publishes his first “guided surgery” system in the inaugural issue of Clin Implant Dent and Rel Research. His system is called “Brånemark Novum” and I think it is the predecessor of all static computer assisted implant surgery we use today. Thanks to a prefabricated surgical guide and drill sleeves, implants are placed in position for immediate loading in the mandible. Thus, another immediacy other than the fresh extraction socket is widely introduced: the immediate loading. Two volumes later in the same journal in 2001 our own Dr. James Chow published some exciting results on immediately placed anterior implants restored with immediate provisional crowns. In a 15 month report on 24 implants, survival was 100%, bone loss minimal and aesthetic results high. Does all this sound familiar? Maybe a little feeling of back to the future? The fact is that immediacy was really hot research topic around the turn of the millenia, including some leading ITI researchers. But then how come it took another 24 years before ITI finally reached a favourable consensus on A1 type immediacy?
Good question…so let’s take a break here to look a bit closer!
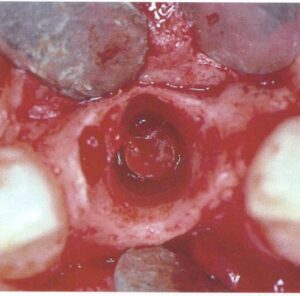
Tissue level implants (some of them hollow cylinder), back then the “ITI system”, were placed in fresh extraction sockets, augmented with GBR and let to heal transmucosally and later be restored with solid abutments. Today I could have considered this impossible, if it wasn’t for a well documented study. The year was 1996, in Bern by Brägger, Hämmerle and Lang. Twenty seven years later, all three were part of the ITI Consensus in Lisbon which accepted A1 immediacy as treatment of choice.
Why were immediate implants so attractive?
Having established transmucosal healing, immediate placement was seen as a natural next frontier. The obvious advantages were reduction of the amount of interventions needed and also the amount of treatment time. Furthermore, immediate function or esthetics was also a significant lure to immediacy, in a time when temporaries and transitional prostheses were mainly removable. There was one more expectation from immediacy, maybe the most promising of all although the least documented and understood: preservation of tissue and in particular bone!
As confidence with immediacy increased, so did the observations of “tissue stability” and “bone stability” multiplied. Steadily, immediacy started to be suggested as the way to counter “atrophy and bone resorption” of the alveolar ridge. Today it might be difficult to understand how this suggestion spiralled into a wider perception through several cycles of self-reinforcement. One has to think that in the early 00’s implant dentistry was still just an outlier practice. The volume of implants placed was a fraction of today’s and the assessment of outcomes mainly dominated by osseointegration and survival. Implant practice was limited to few clinicians, while research was lead by a handful of university centres. Also, the research methodology was limited by the technological means and the knowledge of the time. Assessment of bone margin was limited to what one could see in often poor quality peri-apical radiographs, tissue health was only superficially defined and understood, while peri-implantitis was for many non-existent. With the documented cases of immediacy being limited to the hands of few very experienced clinicians in high profile university clinics and on selected patients, adding a bit of a novelty effect, imprecise technology and tools and there you can see, it does not take much to overestimate the technique, stretch success too thin and stumble.
We are around 2004. The expectations from immediacy peak in the world of implant dentistry, almost as much as the expectations for Olympic medals in Athens. A critical mass of high-profile researchers is convinced that immediate is the way to go to prevent tissue loss and envision immediacy into the mainstream as the new norm. There is a lot of scepticism, but opposition is scarce and criticism rare. The stage is set, for the next move: a breakthrough or a major disaster…
“A bridge too far?”
This classical expression should be well known to all WW2 movie fans, implying how disaster can sometimes loom once success is stretched too far. It was the Allied operation "Market Garden" designed for the liberation of Netherlands, paratroopers were sent behind enemy lines to take over the bridges of Rhine and hold them until the land forces advance to relieve them. The airborne troops managed to take possession and hold the first 3 major bridges (well, almost), but not the bridge of Arnhem which proved to be ...one bridge too far! The unlucky 1st Airborne British division (commanded in the movie played by an amazing Sean Connery) take possession of the bridge only to be pummelled by the constant German counter attacks and lose 4/5 of their men before managing a dramatic retreat.
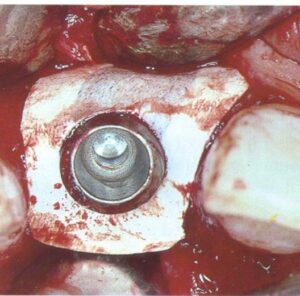
Likewise, the attempt to bring immediacy into the mainstream around 2004 proved to be a bridge too far. The commercial vehicle to materialise the promises of immediacy was soon launched and it was no other than implants designed for placement in extraction sockets aiming to receive immediate provisionals and promising to preserve tissue. Nobel Perfect and Nobel Direct, were two implants launched and marketed as the “immediacy” implants. They were one-piece implants with certain features that were expected to optimise outcomes of placement in fresh extraction sockets. Among these was the provision for a cement retained crown, the lack of an implant-abutment “gap” and also the coronal extension of rough surface, which was envisioned to enhance the attachment of the soft tissue. For this purpose and also to support interproximal papilla, Nobel Perfect had scalloped margins of the rough surface. The spatial positioning of an immediate implant at that time was also not perceived as today; there was a misguided view that filling the socket with titanium was the element which lead to bone preservation. This might be the principle behind another immediacy implant, around that time from Straumann, the TE implant which was a tissue level implant with characteristically wider coronal part.
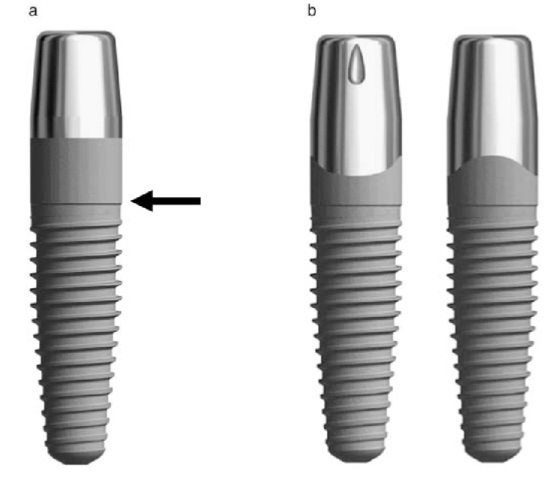
immediacy implants
Nobel Direct (a) and Nobel Perfect (b) were only two of the many implant designs that were introduced for the purpose of immediate placement, about 20 years ago. Since then many designs have followed other are currently being introduced as we speak. As we now well know, not all designs were successful.
The disillusionment
The first hints of the brewing trouble came through the research work of Daniele Botticcelli during 2004-2006, when he was completing his PhD with Jan Lindhe in Gotehnburg. In a series of well-designed animal experiments, they challenged the perception that immediate implants preserve bone and showed beyond doubt how the early bone resorbtion which takes place through the concept of the bundle bone is inevitable and irrelevant to the implant presence or not. The bundle bone is a biological concept which nobody tilll then had seemed to pay much attention to and which in essence was based on the obvious: the periodontal structures develop together with the tooth and they follow it in oblivion after extraction. In some further experiments the same authors introduced some very important parametres of immediate placement such as the “jumping distance”, the position of the implant and the need of augmentation to counter resorption. (Small parenthesis here, tribute to the legend of Jan Lindhe from Gothenburg who I believe is the man still around with the greatest qualitative impact in periodontology and the biology of Implant Dentistry. You might not hear of him that often and you will hardly see his name in consensus papers and guidelines that by now circulate almost annually from different directions. But from the start till the end, he in my mind is the one who more than anyone changed our thinking at critical times with few, targeted, well designed interventions. Parenthesis closed – back to 2004).
After the studies of Botticelli, the debate started to get more heated and opposing camps formed. In the years between 2004-2007 immediacy is being both enthusiastically promoted and increasingly challenged. Then one clinical study comes to finally tip the scale towards the disillusionment. Östman et al 2007 from the group of implantology pioneers Sennerby and Albrektson, documented a chilling realisation: It doesn’t seem to work as we expected… In a clinical study with 48 patients and 115 one-piece implants the clinical outcomes one year after immediate placement and provisionalisation were alarming: Recession and exposure of rough surface was frequently encountered, as well as bone defects filled with granulation tissue, suppuration, dark shades under the mucosa and failures. All in all, the success of the one-piece immediate implants was alarmingly lower than the two piece counterparts.
Back to square 1?
The turning point was reached and the actions that unfolded next in the drama turned the tide completely. In the years that followed, a class action filed by more than 2,900 dentists in US lead to a wide debate that saw in the end the Direct and Perfect implants being discontinued and a settlement for a large sum being reached around 2013. Immediacy, which was just about to hit the wider adoption of the mainstream, was now to be put back to hibernation and return to the safety of confined research centres and expert clinicians for further improvement. We were not back to square 1, but indeed, we had taken quite a few steps back. It is around that time that NP Lang establishes the centre of excellence in implant dentistry in Hong Kong, where immediates will be put on ice for a few years more.
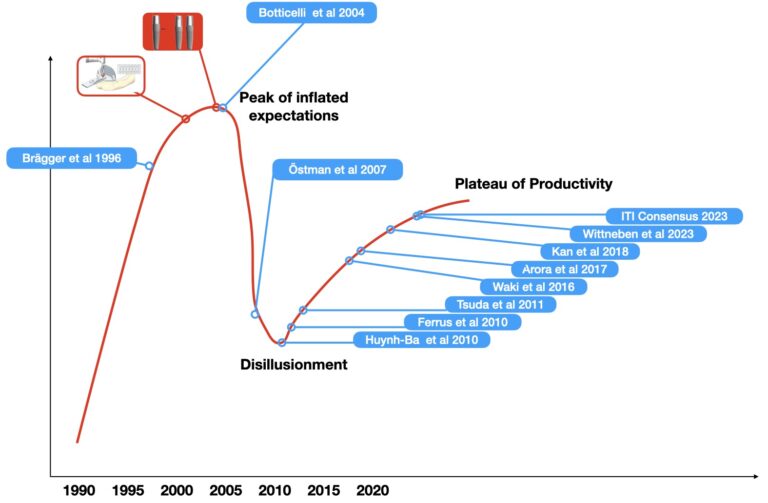
Looking back, we can’t help but recognise a well-known pattern, the Hype Cycle of New technologies, as proposed by the Gardner group. Innovation, comes with a cascading effect: as the first outcomes reinforce our perceptions, expectations rise exponentially from the new protocols, expectations however which are not always founded in solid data. The technology delivers, but the novelty effect and some bias makes our expectations to inflate fast and disproportionally to the actual potential, reaching a euphoric peak just at the point of wider adoption. Then as more and more people jump on the wagon, limitations are becoming more apparent, failures inevitably raise, flawed assumptions are laid bare, mistakes are done and a rapid disillusionment curve crushes down in process painful for many. And there, at the rock-bottom is where reflection starts. Data get scrutinised, questions are being formed, myth is slowly being separated from reality. And the slow progress comes towards the plateau of productivity, where the new technology can now deliver under a better designed and understood realistic framework.
Having hit the rock-bottom in the early 10’s, a slow and well controlled process of research and development was initiated. Carefully designed clinical studies by many groups offered critical insights of the biological processes within immediacy, the tissue reactions that take place and under which parametres. How the bone and the soft tissue truly respond to immediate protocols was deciphered little by little through clinical research of that time around the world. To name only few of the teams that contributed to our new understandind I could mention Pjeturrson and Lang in Bern, Joseph Kan and his team in USA, in Gothenburg Lindhe and his associates, Dennis Tarnow and his team in USA and later also our team in Australia with Saso Ivanovski and many more great teams. In the end, the addition of some critical technologies such as 3D implant planning, CAD/CAM components and Computer Assisted Implant Surgery came to supplement our increased biological understanding and develop the modern concept of “immediacy” which is now an entire workflow, extending well before and after the placement of implants in extraction sockets. Immediacy is again about to hit the mainstream, only now from a very different perspective. But let’s make a pause here.
The critical biological knowledge we have acquired today about immediacy, the technology which binds it all in a single workflow and what is the true potential of immediacy today, these are all topics to discuss in our next article !
References
Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003 Jan-Feb;18(1):31-9.
Kan JY, Rungcharassaeng K, Lozada JL. Bilaminar subepithelial connective tissue grafts for immediate implant placement and provisionalization in the esthetic zone. J Calif Dent Assoc. 2005 Nov;33(11):865-71.
Kan JY, Rungcharassaeng K, Oyama K, Chung SH, Lozada JL. Computer-guided immediate provisionalization of anterior multiple adjacent implants: surgical and prosthodontic rationale. Pract Proced Aesthet Dent. 2006 Nov-Dec;18(10):617-23.
Tsuda H, Rungcharassaeng K, Kan JY, Roe P, Lozada JL, Zimmerman G. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011 Mar-Apr;26(2):427-36.
Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004 Oct;31(10):820-8.
Botticelli D, Persson LG, Lindhe J, Berglundh T. Bone tissue formation adjacent to implants placed in fresh extraction sockets: an experimental study in dogs. Clin Oral Implants Res. 2006 Aug;17(4):351-8.
Huynh-Ba G, Pjetursson BE, Sanz M, Cecchinato D, Ferrus J, Lindhe J, Lang NP. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res. 2010 Jan;21(1):37-42.
Ferrus J, Cecchinato D, Pjetursson EB, Lang NP, Sanz M, Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010 Jan;21(1):22-9.
Kan JYK, Rungcharassaeng K, Deflorian M, Weinstein T, Wang HL, Testori T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000. 2018 Jun;77(1):197-212.
Waki T, Kan JY. Immediate placement and provisionalization of maxillary anterior single implant with guided bone regeneration, connective tissue graft, and coronally positioned flap procedures. Int J Esthet Dent. 2016 Summer;11(2):174-85.
Arora H, Khzam N, Roberts D, Bruce WL, Ivanovski S. Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2-5 year follow up. Clin Implant Dent Relat Res. 2017 Aug;19(4):694-702.
Morton D, Wismeijer D, Chen S, Hamilton A, Wittneben J, Casentini P, Gonzaga L, Lazarin R, Martin W, Molinero-Mourelle P, Obermailer B, Polido WD, Tahmaseb A, Thoma D, Zembic A. Group 5 ITI Consensus Report: Implant placement and loading protocols. Clin Oral Implants Res. 2023 Sep;34 Suppl 26:349-356.
Wittneben, J.-G., Molinero-Mourelle, P., Hamilton, A., Alnasser, M., Obermaier, B., Morton, D., Gallucci, G. O., & Wismeijer, D. (2023). Clinical performance of immediately placed and immediately loaded single implants in the esthetic zone: A systematic review and meta-analysis. Clinical Oral Implants Research, 34(Suppl. 26), 266–303.

8 thoughts on ““Immediacy” revisited: beyond the extraction socket!”
very interesting article, thank you for sharing! Did Branemark have a patent for Novum? what about those who followed?
Interesting question! indeed, I think he did patent Novum, not sure however which part was under protection and if the patent was his. Most likely the patent belonged to the company, either Branemark System on Nobel Biopharma. As Nobel Biocare was later the first one to come with a more sophisticated guided system, maybe the initial patents were already owned by them. Furthermore, although one can protect specific features under a patent I think the implant surgery through a guide as a concept was too wide to be patented, so this might explain why every company at some point came with their own versions…
I find your perspective always very refreshing and analytical! I am only starting now with immediate implants, but it appears there is already so much backgound that I had no idea about! Looking forward to your next article!
I m convinced immediacy is for the benefit of the patient in some cases, still I would prefer to go with early placement in the great majority. Not sure how to see this trend. Thank you for your article, it has been rather illuminating to see this is actually a very old discussion, especially for dentists like me who are now starting with implantology!
You are right, early placement remains the “working horse” even in my clinic, I see however the cases suitable for immediate placement are much more frequent than few years before. I think we are evolving towards this direction and we are getting more confident to use immediacy in a wider array of cases. Still, it has not become the dominant protocol. Early placement has many challenges as well and will help build some advanced skills and understanding. Thus in our professional development I see mastering early placement as an essential step before moving on to immediacy!
Excellent review, thank you for sharing! scientific paradigms and evidence does not always go hand in hand ..!
great article, teh unknown histori behind what we do today is always explain much we do, event if we don’t know!
We should think if in patients not healthy ( diabetic, coronary disease, other metabolic disorders,etc) or people that take anti depressants etc we should go for imediacy or not …is there real good studies about this?