Implant Prosthetic Design and how to "read" it!
by Nikos Mattheos, DDS, MASc, PhD
Martin Janda, DDS, MSc, PhD
Emergence Profile has been among the “hottest” discussions in Implant Dentistry, as it is the feature most connected with long term success and failure. At the same time, it has remained for long an “elusive” concept: an idea that we all think we understand, but we have difficulty to measure, quantify or express in a tangible and objective manner. Some years ago, some pioneering studies attempted to approach this mystical space, describing the concept of Emergence Angle, drawn on periapical radiographs. It opened a pathway, that has lead us today to precise 3-dimensional precision measurements. What does this mean for you and your clinical practice of Implant Dentistry?
Read more below in our recent interview to Dental Diaries!
Can the prosthetic design of an implant prosthesis influence the long-term health of peri-implant tissue?
Yes, it can and this is some fundamental clinical knowledge we have long had from prosthodontics on teeth. Implant Dentistry however has been initially so focused on osseointegration, that it took several decades to awaken to the importance of the prosthesis-tissue interface and how the design of the transmucosal complex can influence both aesthetics and long-term tissue health. This was our main drive to introduce the concept of the Implant Supracrestal Complex some years ago, aiming to study the close interrelation of tissue and components in what we often call as “emergence profile” (1).
The first evidence pointing to this direction came with 3 cross-sectional studies (2-4) which suggested that prosthesis contour of more than 30o -as it appears in peri-apical radiographs- is correlated with increased risk for peri-implantitis in bone level implants. Furthermore, convexity of the prosthesis profile has been correlated with increased recession (5), marginal bone loss (6) and peri-implantitis when combined with overcontouring of the prosthesis (3). This was the first time that there was an attempt to “quantify” elements of the prosthetic design at implants and relate them with pathology. Although these results pointed to a certain direction, it was difficult to extract some concrete suggestions as to what the optimal design should be.
Why was it difficult to come up with specific design guidelines?
Although a tiny anatomical area, the transmucosal part of the implant-abutment-prosthesis is a highly complex structure. Trying to approach this complex 3-dimensional structure solely by means of the 2-dimensional interproximal projection on periapical radiographs is insufficient. Utilising a periapical radiograph to describe the 360o profile of an implant crown, is like taking a screenshot to describe a movie: it only shows one out of the many very different aspects. Furthermore, a major limitation was that the peri-implant soft tissue is not visible in periapical radiographs, thus there was no possibility to relate the crown contour to the actual position and shape of the healthy or inflamed mucosa. The mesial and distal contour was referred to as “Emergence Angle”, but in reality there can be no “emergence” without the soft tissue which the crown is emerging from. Emergence Profile (EP) and Angle (EA) based on the Glossary of Prosthodontic Terms 9th Edition, can only be defined in relation to the “circumscribed soft tissues”, which cannot be accounted for in periapical radiographs. Finally, one of the difficulties with previous studies was that the angles were calculated using “tangent” lines. Geometry defines “tangent” as the line which can be drawn perpendicular to the diameter of a perfect circle, but in the complex and irregular curves of the implant crown a precise tangent is next to impossible to define precisely, seriously limiting the reproducibility of measurements. The tangent line is by definition a “one point” line. In reality, drawn on periapical radiographs the tangents were never “single point”, as one point had always to be placed at the base of the implant platform. We experimented a lot with tangent lines ourselves, even when an expert observer had some consistency, there was always great diversity between different observers. Not to mention that it was next to impossible to communicate to a CAD designer how to design an abutment on the basis of these “tangents”. So although these early studies pointed towards a serious interrelation between prosthetic contour and tissue health, the exact features that affect this relation could not be defined. Also the threshold of 30o is more of a statistical cut-off point that describes the specific sample, rather than a biological fact. We should note that 2 lesser-known cross sectional studies which followed similar methodology did not confirm the correlation of >30o contour and peri-implantitis (7,8).
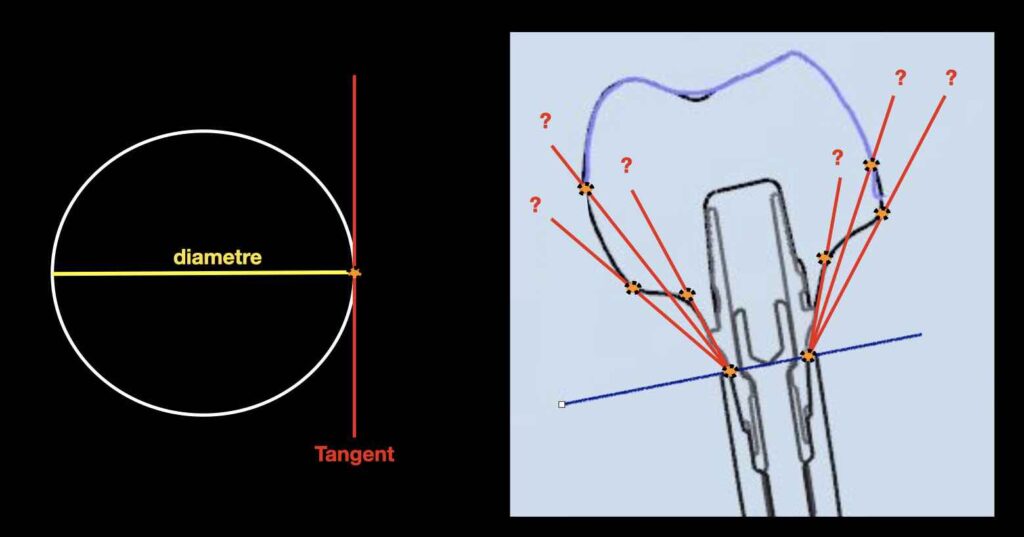
To the left, the tangent as defined reproducibly by geometry, a 1-point of contact line on the perfect circle. To the right, lines that have been drawn to define emergence profile in periapical radiographs: Note that these are always 2-point contact lines, as one point was always placed at the base of the implant. In the complex area of emergence profile, where areas of concavity often follow areas of convexity the lack of standard definition can lead to great difference between different operators.
What new does the recent study bring?
We have thought a lot on the above limitations and we have discussed extensively how we could come up with a methodology that can overcome much of these boundaries.
⇒ The first thing we decided was to move away from the periapical radiographs.
We utilised CBCT matched with intraoral scans, where we could see in detail the full contour of the components in relation to the position, shape and size of the tissue, soft and hard. We then selected eight representative planes for each crown, every 45o , thus we can see the contour from different angles. We excluded the directly mesiodistal plane from clinical measurements, because that is the site under the contact point of the crown, the only site where probing is not possible. It is a paradox that in research we often measure mesial-distal marginal bone loss in peri-apical radiographs and then correlate it with mesial-distal probing depth, when in 3D reality the site of probing and the site of bone loss are sometimes more than 5 mm apart. The digital workflow makes us revisit many of our practices when it comes to precision.
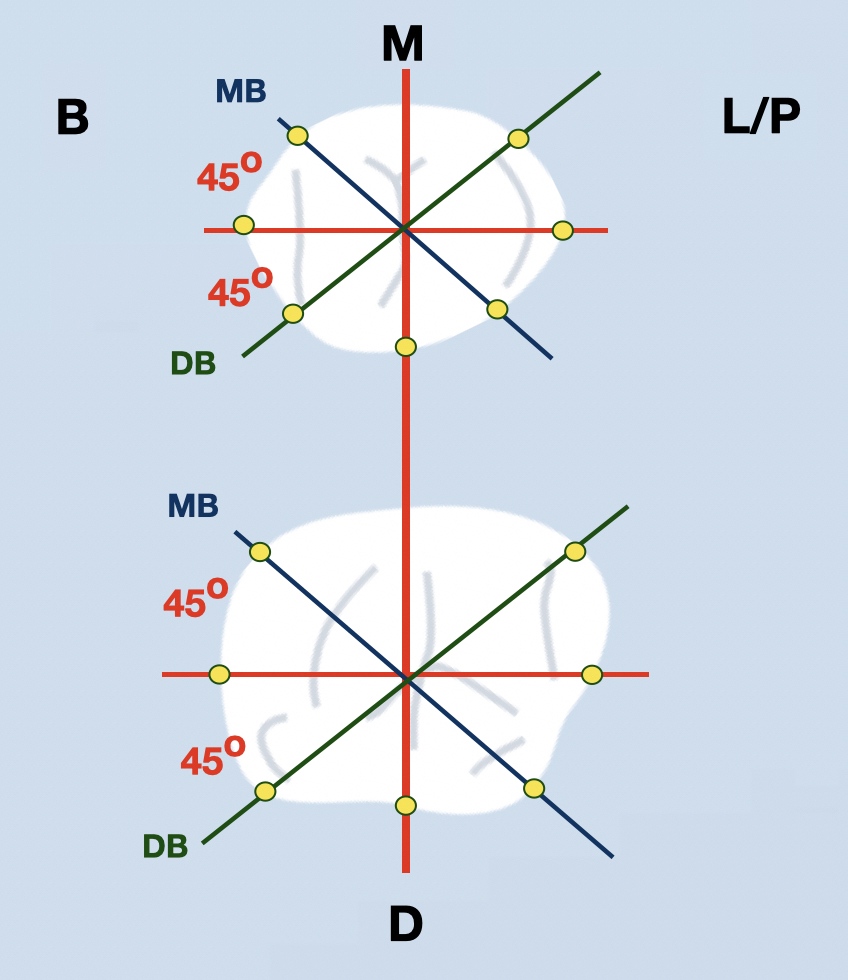
8 precise vertical planes, every 45 degrees
Using the implant axis and the mesiodistal plane, 8 representative planes were defined precisely 45o apart. In each of these planes, two sides of the Implant Supracrestal Complex were represented in a 3-dimensional structure, where tissue and implant components could be precisely visualised and measured.
⇒ The second important decision was to move away from the “tangent” lines. Instead, we used a methodology from Cephalometry, by defining specific and reproducible points and planes, such as the most coronal point of contact between the soft tissue and the crown (true emergence), or the most apical point of contact between the abutment surface and the implant. The methodology was rather complex, we would not get into all details in this brief article as you can read the detailed methodology in the open access publication. In brief, by following a pedantic process of specific planes, points and finally angles we increased precision and reproducibility to the level that two independent observers would come to the same result more than 95% of the times and when not the deviation was still minimal. The importance is not just for the human reproducibility, but also for machine learning. The future is machine-readable only and we clearly needed a system to define objects and conduct measurements which can be identifiable by a CAD automation software. More to come on this soon!
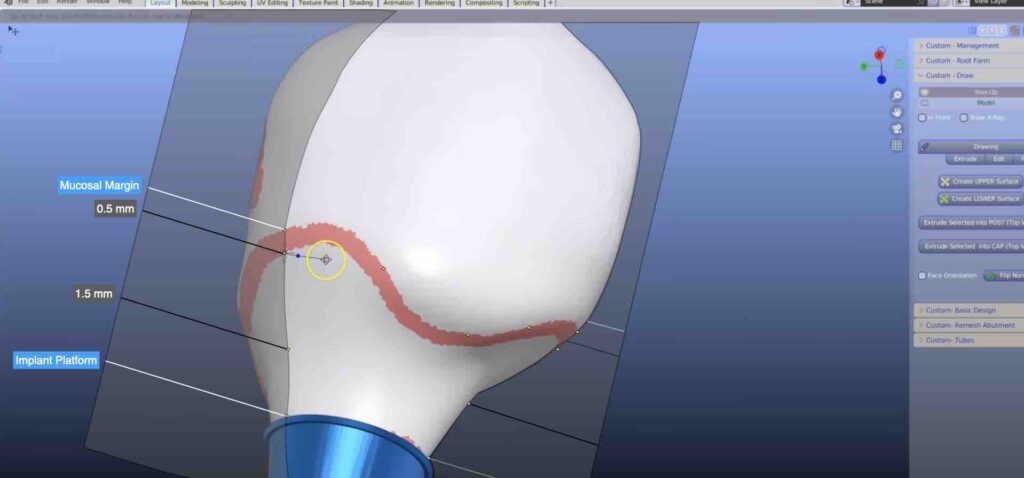
⇒ Finally, we moved away from the “contour” based on a single line. Instead we defined two different angles: The Mucosal Emergence Angle (MEA), the point where the true emergence through the soft tissue takes place and the Deep Angle (DA), at the apical part of the implant supracrestal complex, where the abutment ascents from the implant platform and the bone level. We also measured the total contour angle (TA) as previously done in periapical radiographs as a control.
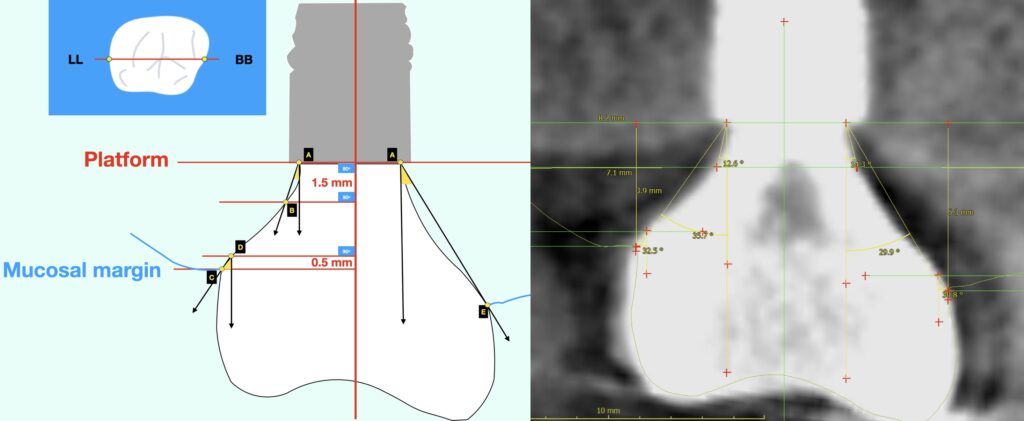
left: Buccal—Palatal slice and definition of 4 horizontal planes perpendicular to implant axis, 5-points (A-E) and the respective 3 angles measured on each side (Mucosal Emergence Angle C-D, Deep Angle A-B, Total Contour A-E).
right: sample of actual optical / radiographic measurement screen.
⇒ Furthermore, we used a patient sample as homogenous as possible: we only included posterior single crowns at bone level implants and we excluded cases where the prosthesis axis was more than 10o divergent from implant axis. We also excluded all probing depth measurements in sites where the crown contour prevented proper insertion of the probe. This is a very important point, as we all know in clinical practice that it is very difficult to probe over-contoured implants without underestimating the probing depth. We ended up excluding about 4% of the measurements, but we have increased this way the validity of the results, by securing that the analysis did not include mistaken or underestimated probing depths. We also used some sophisticated statistics, accounting for three analysis levels: site, implant and patient.
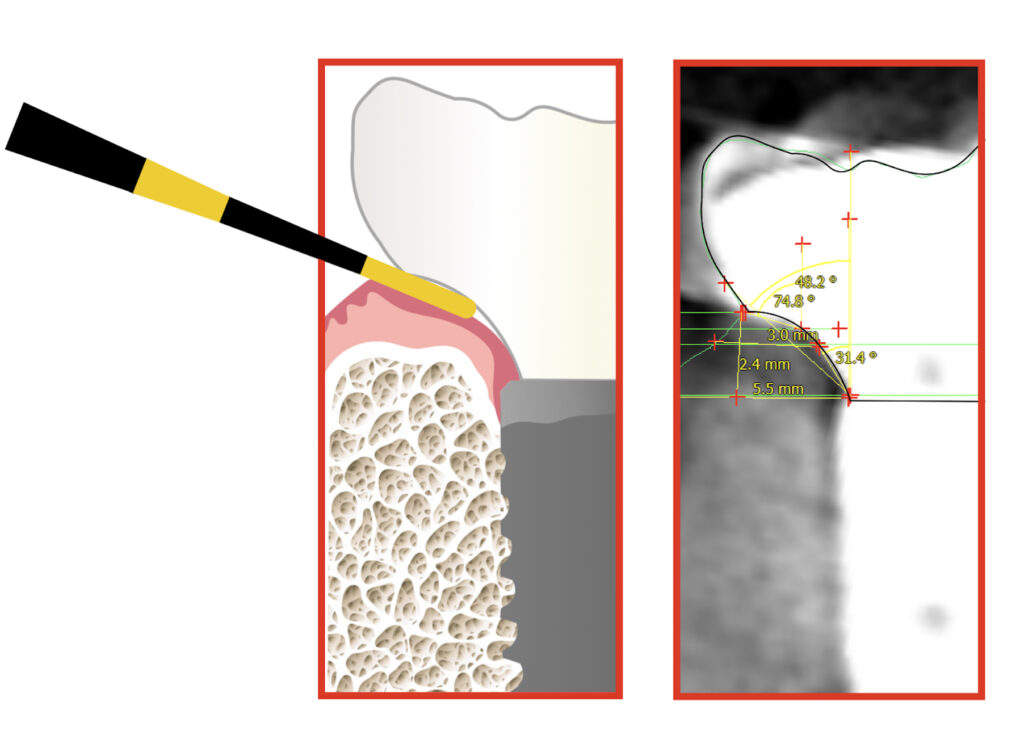
Radiographic image (right) and scematic representation (left) of an actual site where probing depth measurement was deemed as unrealiable, as the overcontouring prevented the appropriate insertion of the probe. The respective Mucosal Emergence Angle at this site was 74.8°.
What was the main result of the study?
The first important finding was – maybe not surprisingly- a very clear and strong correlation of the Mucosal Emergence Angle with inflammation. The risk for inflammation increased in proportion to the widening of the MEA, somewhat slower up to angles of 40o but rising steeper with angles of 50o, 60o, and 70o. As an indication, sites with mucosal angle of ≥70o had 33 times higher risk for bleeding. When all 6 sites of an implant prostheses had MEA ≥ 40o, the risk of having bleeding at all 6 sites was 9.5 times higher. At the same time, no such association was found for the Deep Angle. There was a strong message there: when it comes to inflammation, it’s the emergence that matters, not the entire contour. Thinking of how inflammation starts as a reaction to the biofilm, it makes absolute sense. The deep angle on the other hand is at the bottom of the Implant supracrestal complex, and was not associated with inflammation. This is not surprising either, this area is far from the reach of biofilm at least under healthy conditions. It could be an angle that relates with the early marginal bone loss, or “remodelling” in the short period after the implant placement. But this is something for another discussion.
So what was the main clinical message from the study?
The message is simple, as much as it is powerful: Inflammation starts from the top of the soft tissue. The relation of the implant crown with the soft tissue margin is of strategic importance, as this is the very point of initial plaque accumulation. A narrow angle of the crown at this point will facilitate oral hygiene, 360 o removal of the biofilm and will reduce the risk for inflammation. The wider this angle the higher the risk. Is there a cut-off threshold? I would not think so. Such thresholds are more statistics than actual biological findings. Statisticians typically would choose the number that gives the highest statistical significance and use it as a threshold, e.g. ≥30o, but this does not necessarily reflect a biological phenomenon. In reality, so complex and multifactorial phenomena as inflammation would be more correctly approached by a range, rather than one single cut-off value or an average. Looking at the risk curve we can say that the risk rises mildly from a MEA of 20o to 40o , then steeper towards 50o to 70o. There is no absolute safety zone, but maintaining MEA no wider than 30o-40o is advisable, while the aim should be to keep this angle as narrow as clinically feasible.
And now what next?
This was our first set of clinical data pointing out to the importance of design for clinical outcomes. The data we have compiled from patients included many more parametres, analysis of concavity or convexity, marginal bone levels, detailed tissue measurements. We even got some more ideas while analysing the data. This is the beauty of 3D imaging, once the reconstruction of the implant supracrestal complex is done, the data is saved and can be accessed and measured again and again with different approaches or methods. We are grateful to have the support of a great multidisciplinary team at Chulalongkorn University as well as a multicontinent team of experts, so we are on the way to bring up much more soon! For now you can read the first paper for more details which is available open access thanks to Karolinska Institute and Chulalongkorn University. We are looking forward to your thoughts, suggestions and comments!
Read more at : Rungtanakiat, P., Thitaphanich, N., Chengprapakorn, W., Janda, M., Arksornnukit, M., & Mattheos, N. (2023). Association of prosthetic angles of the Implant Supracrestal Complex with peri‐implant tissue
mucositis. Clinical and Experimental Dental Research, 1–12. https://doi.org/10.1002/cre2.750
Learn the latest news first: subscribe to my blog:
References
- Mattheos, N (b), Vergoulis, I., Janda, M., & Miseli, A. The Implant supracrestal complex and its significance for long term successful clinical outcomes.
Int J Prosthodont, 2021: 34(1) DOI: 10.11607/ijp.7201 - Katafuchi M, Weinstein BF, Leroux BG, Chen YW, Daubert DM. Restoration contour is a risk indicator for peri-implantitis: A cross-sectional radiographic analysis.
- J Clin Periodontol. 2018 Feb;45(2):225-232. doi: 10.1111/jcpe.12829.
- Yi Y, Koo KT, Schwarz F, Ben Amara H, Heo SJ. Association of prosthetic features and peri-implantitis: A cross-sectional study. J Clin Periodontol. 2020 Mar;47(3):392-403.
- Majzoub J, Chen Z, Saleh I, Askar H, Wang HL. Influence of restorative design on the progression of peri-implant bone loss: A retrospective study. J Periodontol. 2021 Apr;92(4):536-546
- Siegenthaler M, Strauss FJ, Gamper F, Hämmerle CHF, Jung RE, Thoma DS. Anterior implant restorations with a convex emergence profile increase the frequency of recession: 12-month results of a randomized controlled clinical trial. J Clin Periodontol. 2022 Nov;49(11):1145-1157. doi: 10.1111/jcpe.13696.
- Valente, N., Wu, M., Toti, P., & Derchi, G. Impact of Concave/Convergent vs Parallel/Divergent Implant Transmucosal Profiles on Hard and Soft Periimplant Tissues: A Systematic Review and Meta-Analysis. Inter J Pros 2020:33(5):553-564.
- Lops D, Romeo E, Stocchero M, Palazzolo A, Manfredi B, Sbricoli L. Marginal Bone Maintenance and Different Prosthetic Emergence Angles: A 3-Year Retrospective Study. J Clin Med. 2022 Apr 4;11(7):2014. doi: 10.3390/jcm11072014.
6 thoughts on “Implant Emergence Profile Demystified”
Very interesting, thank you for sharing!
thank you for this article! So if I may ask what is your advice if probing is not possible around an implant crown? I guess it’s easy to “exclude” the patient in a study, but in real life when you have a patient in the chair and you see that probing is not possible, what do you advice?
many thanks, Martin
Your approach is very analytical indeed! In practical terms however, there might be challenges, for example to prefer a wider implant to make a better profile or a more narrow that reduces the need for augmentations for example. How do you choose?
many thanks for sharing your knowledge so generously!
Wen Yang
Thank you for your kind comment! indeed, in real life the clinical decisions are never easy and we have to combine many factors, from the patient the design or the anatomy. the ideal profile is sometimes not feasible and some compromise has to be reached. I think the important think is to be aware of all the different risks and make a conscious choice if you have to introduce a compromise somewhere. A narrow implant will reach primary stability easier in compromised bone or maybe save the need for augmentation, but maybe with somewhat deeper placement we can also improve the emergence profile. In other cases this might be not feasible, so at least by knowing all factors we can chose the area of least risks to compromise. Also not all patients are the same. Some patients with low risks or high motivation and dexterity might be able to maintain implants with sub-optimal design through careful oral hygiene. I think in the end, it is our clinical judgement that has the last word. We start from identifying the optimal and if not feasible, see what discounts will bear the least risks! Thank you for your thoughts! N
Thank you for this thorough analysis. It is interesting to see that the mucosal emergence angle is the more important to consider since it is the angle with more effects on peri-implant health.
My question is, when designing a prothesis, it is better to contour the deep part with more divergent angle so that when going coronally, we can achieve a shallower mucosal and total emergence angle. This however results in a convex contour (as apposed to the first figure explaining the tangent line where the deep angle is shallower than he total angle in the case of a prothesis with a concave profile). In this case, a convex profile would be actually beneficial?