From the very start of my training in Periodontology, I learned to see my probe as an Ultimate Judge. Three interchangeable lines – the magical reading of “3mm” – could split the world in two: sickness from health, success from failure, sulcus from pocket. Then implants came, and suddenly the picture blurred. Having spent years considering everything deeper than 3mm around teeth as disease, I was shocked to realise that I was now daily creating deep probing depths around implants …
…but let’s take things from the start!
The sulcus is one of the first things you would remember from the early days of your undergraduate years. This tiny “slot” between the tooth and the gums, usually measured between half to one-and-a-half millimetre. Later on in your studies you might have come across the sulcus as part of the “Biologic Width”, a concept that I found certainly much more complex to grasp as an undergraduate. Was the sulcus truly part of the Biologic Width around healthy teeth? That was the content of some academic discussions back then, but then again it didn’t matter, because – unlike implants- the depth of the healthy sulcus around teeth is
genetically determined and rather consistent. Then implants came…
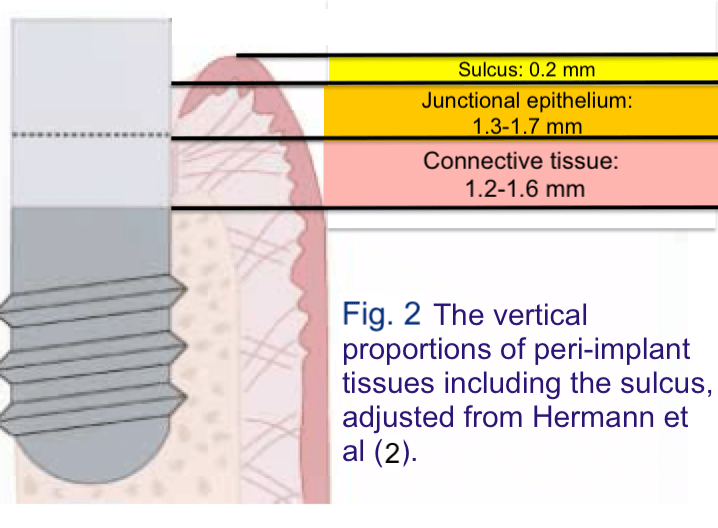
Originally with implants, the focus was in the bone, but soon the peri-implant soft tissue came under the scrutiny of research. Landmark histological studies such as the ones by Berglundh et al (1) compared the soft tissues around teeth and implants and identified similarities: the Connective Tissue zone, the Junctional Epithelium and Sulcus around implants amounted altogether to 3,8mm in vertical dimension, as opposed to 3,17mm around teeth (Fig. 1). Later studies reinforced these results, further measuring the sulcus around implants to be between 0.2-0.3 mm such as the study by Hermann et al (2).
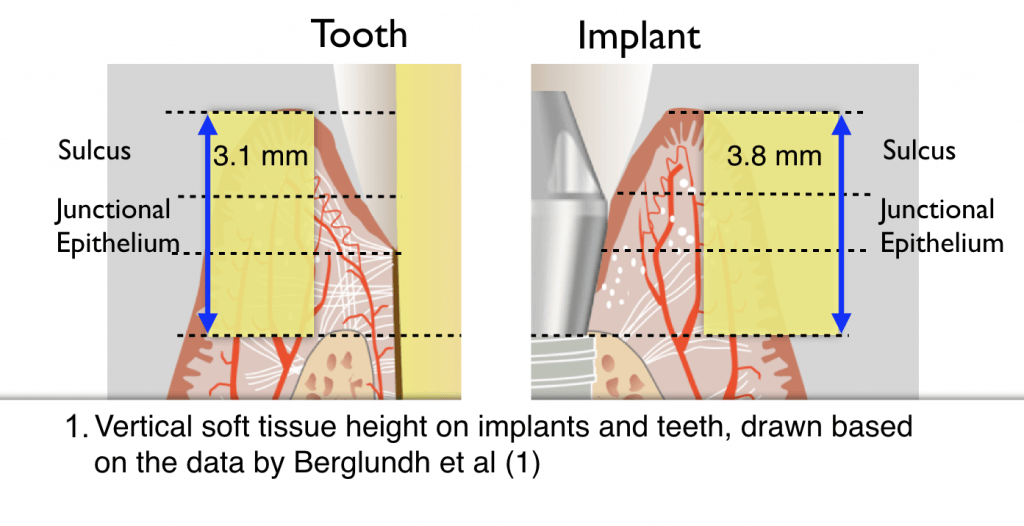
In both cases the peri-implant sulcus was consistently shallow. Influenced by the dominant teeth-based paradigm of the time, the sulcus together with the Junctional epithelium and the Connective tissue were defined as the peri-implant tissue Biologic Width. (Fig 2)
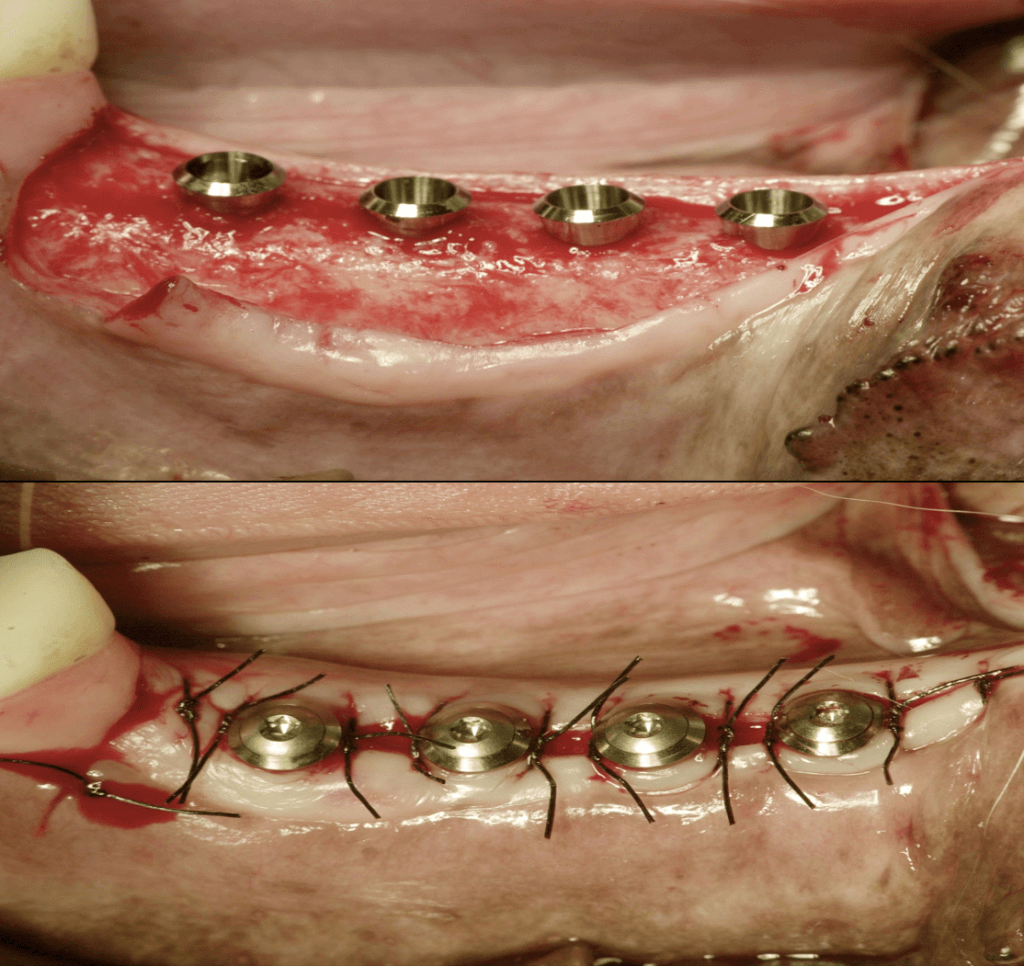
A critical detail however was that both studies were conducted on dogs. I’m sure that most of you never had a Beagle dog in your practice requesting an implant, so please take a look at the typical anatomy of the sites that received implants in Fig 3. What you see is an abundance of flat, wide alveolar bone, covered by consistently thin and flat oral mucosa. When sutured around tissue-level implants, it is no surprise that it will result in a consistent soft tissue height with a consistently shallow sulcus.
The sulcus depth in these sites was only such because of the specific anatomic conditions, rather than any universal biological pattern or any predetermined ratio between the different tissue components.
Overseeing this fact, resulted in a widespread and long-lasting misunderstanding:
The term “Biologic Width” was established mixing two very different things: a genetically-determined attachment zone with an anatomy-specific zone
The connective tissue and the junctional epithelium constitutes a genetically-determined zone, which as of today, we have not managed to predictably manipulate. It appears to establish itself in a more or less similar pattern and size, regardless of implant design, surface or surgical protocol.
The sulcus, however, is a whole different story: its depth is mainly determined by the local anatomy, the availability and consistency of the soft tissues and the depth of implant placement.
In other words, the peri-implant tissues are divided into two different parts: one that is determined by genetics and biology and another that is primarily determined by local anatomy and the operator, his protocols and technology.
How does this difference affect our decision making and strategies in implant placement? Well, that is something I would like to discuss in more detail next time…!
Coming Next: in part 2:
Biologic Width or Supracrestal Attachment?
– The Peri-implant sulcus in anterior and posterior implants: Friend or Foe?
References
- Berglundh T et al. The soft tissue barrier at implants and teeth.
Clin Oral Implants Res.1991(2):81-90. - Hermann JS et al. Biologic Width around one- and two-piece titanium implants. Clin Oral Implants Res. 2001 (6):559-71.



6 thoughts on “Who’s afraid of the deep bad Sulcus…? (part 1)”
Supеrb, what a blog it is! This website provides valuable information to us, keep it up.
many thanks for your kind feedback!
Hello Dr.Mattheos,
Greetings from Germany! As you must have already received a ton compliments for the MOOC, let me start by saying thank you from the bottom of my heart 🙂
I am a (relatively) young dentist (BDS) from India, now practising in Germany. Although I have attended many Implant courses in Germany, diplomas n now Masters, none of them bothered to solidify the basics like your course did. Also most of the mentors are just interested in bragging about their own cases, rather than teaching the fundamentals.
Is there any way to study more with you? As in an extensive online Masters course with maybe few hands-on Modules? I wish I could find a Mentor like you , Sir, here :((
Best regards,
Dr.Priya Sharma
Dear Dr. Priya,
thank you very much for your kind interest and trust! I wish you a great start in the new year and I hope there will be opportunities to meet and discuss more on Implant Dentistry in the near future! Please keep an eye on the page for upcoming courses and education events and you can also contact me at https://www.facebook.com/DrNikosMattheos/
best regards
Nikos
Spot on with this write-up, I absolutely feel this web site needs a lot more attention. I’ll probably be returning to see
more, thanks for the info!
Generally I do not read article on blogs, however I wish
to say that this write-up very pressured me to check out and do so!
Your writing taste has been amazed me. Thank you, very nice post.