Why we combined static and dynamic guided implant surgery and what did we learned from this!
by Nikos Mattheos, DDS, MASc, PhD and
Atiphan Pimkhaokham, DDS, PhD, FRCDT (OMFS)
Computer Assisted Implant Surgery is best known as static or dynamic guided surgery. Static utilises a 3d-printed surgical guide a special drilling set, while the dynamic relies in a real-time tracking system to direct the surgeon. Both systems have their own potential and limitations, but have achieved comparable results.
…but what if we were to use them both at the same time?
Computer Assisted Implant Surgery (CAIS) can help us achieve highly precise implant placement and that is by now a fact well established by more than 200 clinical trials. Either as static or dynamic, guided implant surgery can reduce the deviation of the implant platform at placement to about 1mm or less on average as has been assessed in multiple clinical scenarios from single implant to fully edentulous patients.
Although CAIS has significantly improved accuracy of implant placement in comparison to freehand surgery, all studies have shown comparable clinical outcomes for static and dynamic systems. Furthermore, neither static nor dynamic have completely eliminated errors. However, as static and dynamic CAIS systems utilise very different technologies and workflow, it becomes apparent that each has its own limitations and suffers from different sources of error.
What are the most common sources of error for each?
Fit and stability of the surgical guide is probably the most important source of error in the static CAIS. Furthermore, the material used and the manufacturing protocol of the surgical guide can allow for different extent of elasticity. Depending on the operator’s ergonomic position, patients’ anatomy, mouth opening and the implant site, the “leeway” between sleeve and drill and the elasticity of the guide might allow for deviation towards specific directions. Even the actual design of the guided surgery implant system can also influence clinical accuracy. Static CAIS tends to have more “systemic” influence on accuracy, as an inaccurate guide will affect all implants placed in the case of multiple sites. Dynamic CAIS on the other hand does not require the use of a guide, so it eliminates such a “systemic” influence. Still, accuracy can be affected by other systemic sources of error such as calibration and system configuration, registration of the drills and implants, interruptions in signal transmission or operator’s experience and learning curve.
As the limitations of each technique differ, could we increase accuracy by combining both static and dynamic in the same procedure? Could the combination of the two compensate for each other’s deficiencies and increase accuracy of implant placement beyond the current standards?
We tried this for you and here we come with some answers!

The use of the combined techniques is relatively simple if one has experience with both. At the left: the registration of the handpiece. Middle: registration of the drill tip and right: drilling with the surgical guide in place (right) and the splint with the fiducial markers of the dynamic navigation system (left).
Looking for the answer!
We conducted a randomised clinical trial with 120 patients who received a single implant each. All implants were planned virtually in the same way, then patients were randomized in 4 groups: Static alone, Dynamic alone, Static and Dynamic combined and a Control group, where the implant was placed freehand.
How can you combine static and dynamic? Well that was not too difficult actually. In principle, you have to follow the workflow of the static, print the guide accordingly and then register and calibrate the guided surgery drills for the dynamic CAIS before the surgery. In the surgery the operator will place the surgical guide and continue with the drills as usual, only now with the visual aid of the correct angle and depth also displayed in real time.
Now, one might wonder if this setup really makes sense, as you cannot modify the position of the implant through the surgical guide. Well, you actually can. Remember we said that one common source of deviation is the elasticity of the surgical guide, combined with the “leeway” or gap between the sleeve and the drill and the operator’s ergonomic position. Now using the dynamic system helped realise such an error in real time and compensate for it. We found that particularly important in correcting the angle. You see, the leeway of the surgical guide can still allow for angle deviation of as much as 7-8 degrees, even when the drill has reached its final depth, without the operator being aware of it. By visualizing this error, the operator could correct accordingly thus reducing significantly the final deviation.
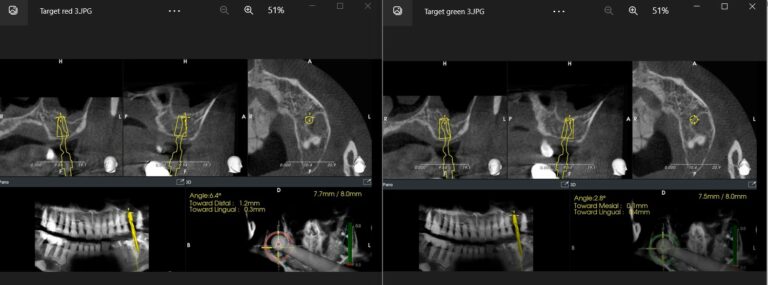
To the left, the implant drill is almost in it’s final depth (7.7/8 mm) yet the angle deviation is at 6.4 degrees. Seeing the red indicator in the navigation system, the operator can now correct the angle accordingly, until the indicator turns green (right side, angle corrected to 2.8 degrees)
Correcting the angle is actually a very important parametre. In reality there are only two main parametres in 3-dimensional deviation of the implant position: platform and angle. We also measure the deviation at apex, but in reality this is a surrogate of angle deviation: It amplifies the deviation at platform by the implant length. The bigger the angle deviation and the longer the implant, the bigger the apex deviation would be. But for 0 degree angle deviation, the apex deviation will be exactly as much as the one in the platform and this is elementary geometry.
there are only two parametres in 3-dimensional deviation : platform and angle. Deviation at apex is just a surrogate of angle deviation.
And what did we find?
The final result: combining static and dynamic CAIS lead to the smallest deviation recorded so far a mean 3D platform deviation of 0.62 ± 0.50mm, which was some 40% less than the average 1 mm we could get with static or dynamic alone. In terms of angle, the mean was 1.24 ± 1.41, which was about half of the average 3o that static or dynamic alone would offer. Maybe the most important was actually to study the frequencies, rather than the average, and there one could see that the combined static and dynamic had achieved a significant portion of the placements with an ultra high accuracy, at least when compared to other methods. You can read more details in the recently published study by Yotpibulwong et al in Clin Oral Impl Res 2023.
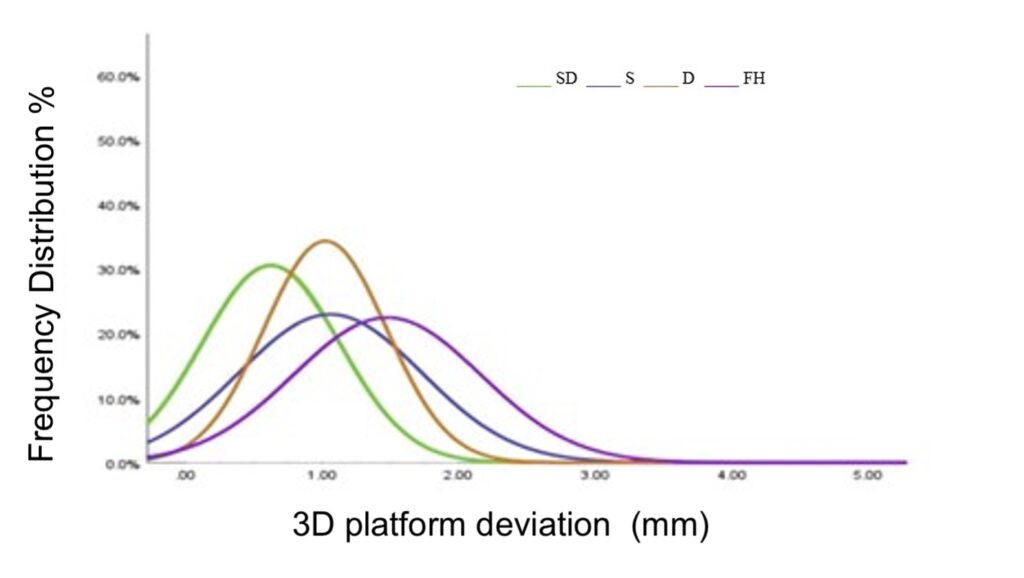
Observe with the green curve the frequency distribution of the deviation at platform for the combined static and dynamic surgery. Having most of the observations left of all other curves also implies that in more than half of the cases the accuracy achieved was below the threshold of 0.8 mm. Interestingly, although static (blue) and dynamic (brown) alone have similar average, the dynamic appears less spread, possibly indicating more cases within a set of acceptable deviation.
So what does this result mean for our clinical practice?
Exciting results at least from a statistical point of view, but of course one might have multiple readings. It was true that by combining two cutting edge technologies in the hands of experienced operators we could push the margins of accuracy even higher. It remains also true that despite the best of our efforts, we could not eliminate the biggest part of the deviation. It appears that somewhere there between the 0.65 and 0.75 mm lies the “hard core” of the “systemic” or workflow cumulative error, which is no longer influenced by the actual surgery. Discrepancies in the algorithm of the CBCT, the STL and the treatment planning software that renders everything, imprecisions in the design or the 3D printing of the guides as well as limitation of our own measurement methods, it can all add up to an error difficult to further suppress.
The combination of the two could bring implant placement to the highest level of accuracy seen so far, but how important would this be in clinical terms? Although increased accuracy is always desired, the costs related with combining the static and dynamic CAIS should not be ignored. Cost/effectiveness would be the main determinant and it would require assessment of different clinical scenaria and multiple aspects of the treatment such as costs, surgical time, safety, healing, patient related outcomes and more.
Not surprisingly, to get the average deviation down from 1 to 0.7 mm would require twice as much the costs and effort it took to get it from 2-3mm to 1mm, with either static or guided alone. For most clinical applications, the average deviation of about 0.9-1mm could be sufficient. On the other hand, in extensive and complex procedures such as for example in cases of immediate implant placement and restoration with pre-fabricated prosthesis the increased 0.2-0.4 mm of accuracy might be worthy investment.
Technology is evolving fast and new frontiers are being constantly opened. With regards to accuracy of implant placement with CAIS, I think we have reached the borders of the current technologies. It would take some out-of-the-box development to push accuracy drastically higher. But beyond accuracy, there are many frontiers waiting to be explored when it comes to computer assisted implant surgery…!
Moving on..!
Hear the latest news first: Subscribe to my newsletter!
References
1. T. Yotpibulwong, S. Arunjaroensuk, B. Kaboosaya, P. Sinpitaksakul, M. Arksornnukit, N. Mattheos, Atiphan Pimkhaokham. Accuracy of implant placement with combined use of static and dynamic Computer Assisted Implant Surgery in single tooth space: a randomized controlled trial. February 2023. Clinical Oral Implants Research
DOI: 10.1111/clr.14043