Deciphering Personalised, Preventive, Predictive and Participatory
by Nikos Mattheos, DDS, MASc, PhD
Precision Medicine or P4 is a paradigm of care which considers a patient’s individual characteristics to guide diagnosis and treatment… but wait a minute, isn’t this what we have always done? Isn’t this the reason we have to take medical history, do lab tests and dig into the patients background? Indeed it is. But then what’s all the fuzz with P4? Is P4 so different to what we have conventionally practiced? It is. But half the buzz is in the mindset, the other half in the technology. And as Implant Dentistry matures as a digital workflow, P4 is now waiting at the doorstep of your clinic!
How can this new paradigm impact your practice?
Precision medicine is a paradigm shift in medical care that is increasingly applicable to all disciplines. You might have heard it frequently as a buzzword, but in essence Precision Medicine considers a patient’s individual characteristics to guide diagnosis and treatment. But wait a minute, isn’t this what we have always done in medicine? Isn’t this the reason we have to take medical history, do lab tests, ask and dig into the patients background and experience? Indeed it is. Medicine has been striving to be personalised since the time of Hippocrates who famously said “It’s far more important to know what person the disease has than what disease the person has”. But then if we can credit Hippocrates with practicing precision medicine, what’s all the fuzz with P4? Is P4 so different to what we have conventionally practiced? It is. But half the buzz is in the mindset, the other half in the technology.
"It's far more important to know what person the disease has than what disease the person has”
....said Hippocrates, about 2500 years ago. If only he also had omics available back then!
P4 and Implant Dentistry
So does Implant Dentistry come in play with P4? Of course. Implant dentistry is very well placed for the P4 paradigm, as possibly the most widespread and one of the most successful applications in rehabilitation medical care. But it only starts to make sense when the conditions mature, that is when the technology utilised is ripe enough to support P4. And what technology was that? Remember the catalysts: Digital Technologies and Big Data. When the practice of implant dentistry migrates to a fully digital workflow and large numbers of data accumulate in digital formats, P4 becomes a new convenient habitat. Four keywords describe this in full: Personalised, Preventive, Predictive and Participatory. Now how does these apply to Implant dentistry?

Personalised:
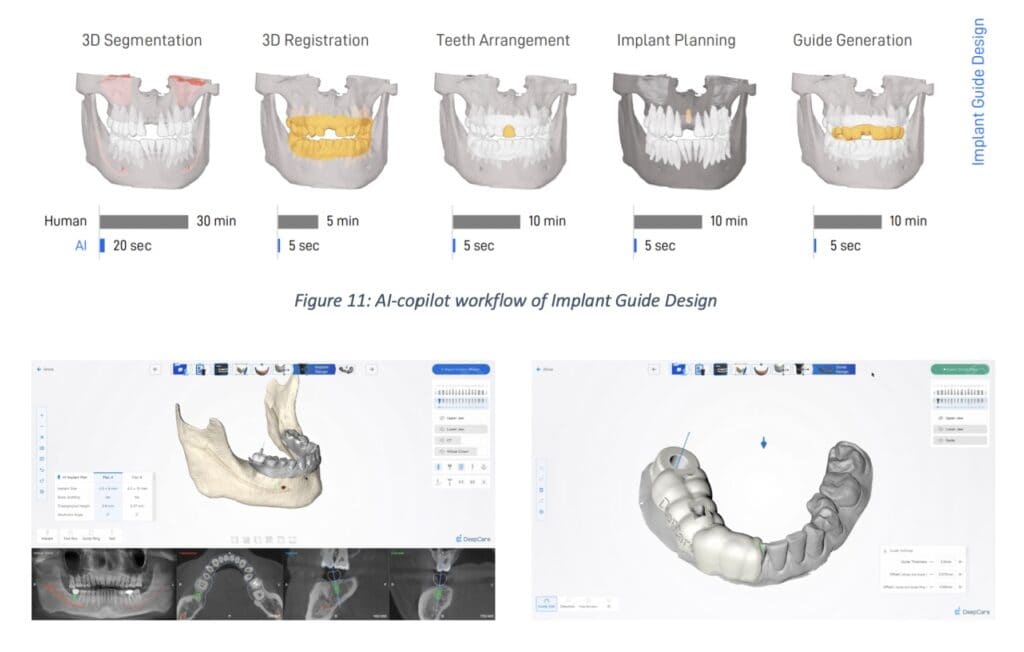
Personalisation is the key of concept of Precision Medicine, and it is nothing new in implant dentistry either. However, with a fully digital workflow we can now push the boundaries to a whole new level. 3-dimensional imaging data are collected from CBCT and surface scans, then compiled into a full anatomic representation in a Computer-aided Design Implant Planing Software (CAD-IPS). Personalised prosthetic components can be milled or 3d printed, while the surgery, another critical step is now also personalised, by exporting the treatment plan to a d-CAIS or navigation surgery system. By he time the treatment is completed we establish a digitally documented baseline, having reached a fully tailor-made implant treatment, including components and workflow, empowered by CAD/CAM and guided surgery.
Preventive
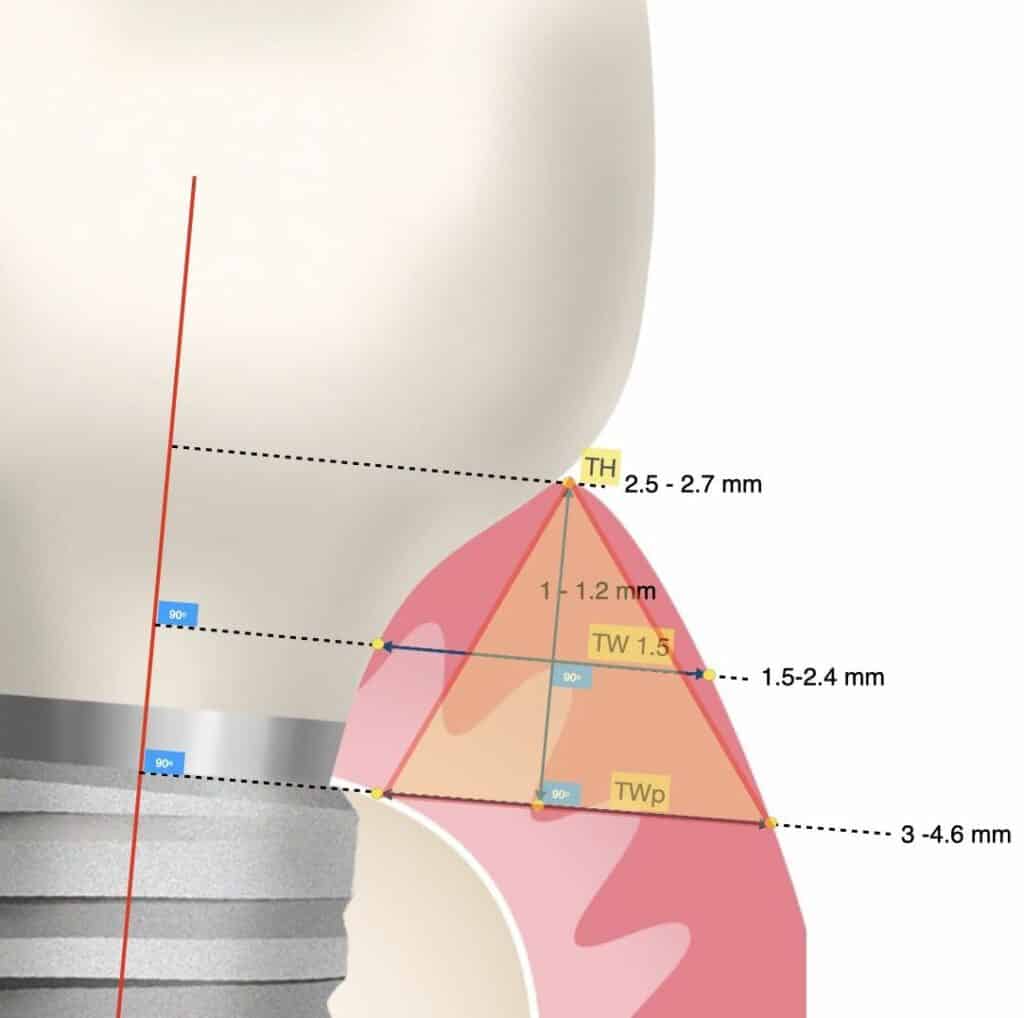
With our ability to design precise and tailor made treatment components also increases our understanding of the design implications to long term clinical outcomes. From the first study which showed the implant prosthesis contour in periapical radiographs to be associated with peri-implantitis in 2018, a large volume of studies using 3-dimensional data have come to point out design elements which can act preventive or predispose to problems in the long term. What used to be a vague reference as “Emergence Profile” is now understood as a complex man-made system, where tissue, components and bacteria synergise and antagonise to determine disease or health. Today it is clear that “design matters”! Applying the evidence-based design principles in the digital treatment plan, together with all other personal parametres is essential for preventing long term problems in implant therapy.
Predictive
This concept is entirely new in a way. In the past, our prognostic ability was purely based on Biostatistics, which is a computation model that allows predictions on a population basis. Analysing data from clinical studies, biostatistics would allow you to estimate the probability of an event to a population under treatment. The more parametres studied and the larger the sample , the better would be the ability of the biostatistics to support clinical decisions. However the last leap of faith in interpretation was always on the clinician, who had to use his judgement to decide which side of the probability lies the individual patient on the chair.
Predictive models have been revolutionised by machine learning. Machine learning includes computational models which are fundamentally different to biostatistics, as they are designed to give predictions for the individual, instead of the population. This doesn’t have to be “prediction” in the sense of guessing the future, AI models treat prompts as problems, and respond by “predicting” the most suitable solution which could be a text, image, video, design etc. This individual predictive ability would revolutionise the digital treatment planning. For example, as AI powered CAD software would perform segmentation of all different tissue and registration of all 3D files (it’s here!), or propose an evidence-based, preventive prosthetic design matched to the individual patient’s anatomy (it’s coming!).
You might hear of some predictive applications closer to he actual use of this word about guessing the future. For example, studies have developed ML models aiming to predict the primary stability or the 5 year survival of implants. I am less excited about such models however. First, because none of these claims has yet been shown to work in clinical tests and second because judging from how these models have been trained, I very much doubt these predictions will be meaningful in clinical settings. Maybe some other time we can discuss the serious limitations of training models on selected retrospective and downsized data. Finally, to be honest, this is not the problem I need AI to solve for me. I believe I have good enough aids in my digital treatment plan to foresee cases where implant stability might be challenging and mitigate this risk. Predictive algorithmic automation based on machine learning models is an expensive and resource intensive process, which however has great potential in implant dentistry, to automate repetitive procedures and also resolve real problems.
Participatory
This is all about empowering the patient to share the decisions and responsibility of the treatment. Again, this is nothing new in implant dentistry. However, the digital tools can push the boundaries of possibilities we have to educate our patients and to simulate and communicate treatment outcomes that were only left up to imagination in the past. Personal treatment outcome simulation is becoming increasingly accurate, while the treatment baseline can become by a “digital twin”. Future examinations and automated comparisons can help us get timely feedback and warning of any changes, while patients’ self-monitoring technology is now increasingly available for oral health.

P4 is here to stay
To sum up, like with all new paradigms, Precision Medicine is nothing entirely new, but rather the evolution of old concepts catalysed by new tools. It is however a paradigm that makes sense in today’s benchmark of clinical practice and something that will be increasingly required as a standard of care by our patients. In the near future, the 4Ps Personalised, Preventive, Predictive and Participatory will be keywords that all our implant treatments will be weighted against. And to close by quoting Jack Sparow :
“whoever falls behind, is left behind”.
But not you 🙂



4 thoughts on “Precision Implant Dentistry?”
Very interesting concept, thank you for sharing this! P4 has never before been explained like that! A bit confused though with the AI and the predictive approach, why you think it would not really work for predicting longevity or success of the implants?
I have recently seen an AI powered segmentation module, looks good but not sure how much is commercial claims. Then again, I already use a planning software. I have been buying many gadgets over time, I’m sure most dentists think like that, but with software is more tricky, time to learn is my main concern. and what if in the end it doesn’t seem to deliver…Wasting money is one thing, wasting time I think huts more! Not sure if worth investing. What is your view?
Thank you for your comment, indeed it reflects my thoughts too.. Too many tools are being developed and marketed and many are based on great ideas, but my main concerns is the limited interoperability. I struggle to keep my workflow streamlined, with as little steps as possible, reduce uploads and checks and exports ad conversions. In the end I have thought I might be willing to accept a system that takes me to the desired outcomes with less steps, than a seemingly optimal workflow, which however requires jumping from one to another software. Maybe this is what manufacturers try to do with denying interoperability, lock you in an “apple style’ environment, but it cuts both ways and you might end up refusing a good product all together because it does not allow you to use a specific software or device at some step…difficult one this one and no solution that I have ready…
Thank you for this critical look, great to see someone also things that personalised medicine was not discovered today!