Part I: Periodontal vs Peri-implant tissue: Thinking like an architect!
by Nikos Mattheos, DDS, MASc, PhD
Architecture is an art and we often see impressive designs of houses that look fancy, curious or exciting. Still, to withstand forces of nature and fulfill the needs of those who live in it, a house must primarily adhere to certain less fancy principles, static rules, dimensions and proportions. In that sense, peri-implant tissue as part of a designed system – the implant supracrestal complex- might not be different to any architectural design. We might be tempted to get fancy, but in the end, the clinical outcome might be restrained by some overriding rules of dimensions and proportions.
So how can this help you next time you plot the architectural blueprint of a new implant treatment?
Periodontal & Peri-implant tissue: Same- same, but different...!
For decades the comparison between periodontal and peri-implant tissue has been the subject of endless discussions and many studies. Focus has moved in different directions, from comparing dimensions to studying differences in microanatomy, vascularisiation, fibrous components and structures. Thanks to many studies, today we understand very well the similarities and differences in the microanatomy and physiology of the two tissues. Taking a step back however and looking from afar, there is a fundamental difference between them: Periodontal tissue is a physiological tissue, while peri-implant mucosa is a repair tissue. Both unique – both different!
Now let’s take a pause here to look deeper in this! Both periodontal and peri-implant tissue are created in response to a specific but very different stimulus: the emergence of a natural tooth for the first and the surgical implantation of a mechanical device for the latter.
The first, periodontal tissue is created following a physiological event, the eruption of a natural tooth, which it follows at all stages as directed by millions of years of evolution. In the end, the periodontal tissue resumes a final morphology that closely corresponds to the anatomy of the original cause: the natural tooth, fully supported by the corresponding vascularisation and physiology. Thus the “architectural blueprint” of the periodontal tissue is directed by strict proportions and dimensions supplementary to the natural tooth, like two branches that grow together from the same seed. Abnormalities of tooth morphology are also reflected to irregularities of the periodontal tissue.
The peri-implant tissue is not created following an orchestrated physiological stimulus, but rather a trauma: surgical cuts, bone drills, tissue damage and the final implantation of a metallic system. The physiological process of tooth eruption that takes years and a highly orchestrated hormonal environment to materialise, is being imitated by a 30 minute surgery. It’s like cutting down one of the trees that were growing together in the paragraph above and building a concrete wall in its place. The remaining branch will survive but eventually adhere to or get limited by the shape of the wall, continue to grow at the space the wall directs. Like periodontal tissue, peri-implant tissue will also adopt to match its cause, in this case however the response will be directed by immediate repair and sealing needs, rather than a long physiological process. The result can serve our basic needs albeit…same-same, but different!
Peri-implant tissue Rule Nr. 1:
For years we’ve been playing with 3D morphological measurements of the entire implant supracrestal complex and emergence profile, trying to decipher patterns that link design elements with biological outcomes. Some of our findings helped us gain new insights, like for example how prosthesis emergence profile is strongly related to the risk of mucositis and which particular design elements are responsible for this increased risk. Other findings are still puzzling us and some keep us awake (some) nights, trying to design better studies. Recently we also started to feed in all these data to machine learning models, albeit without some groundbreaking discovery as of yet (but more coming soon!). In such a multifactorial environment, few findings could reach the consistency to even come close to a “rule”, even a rule of the thumb… until one did!
A consistent finding:
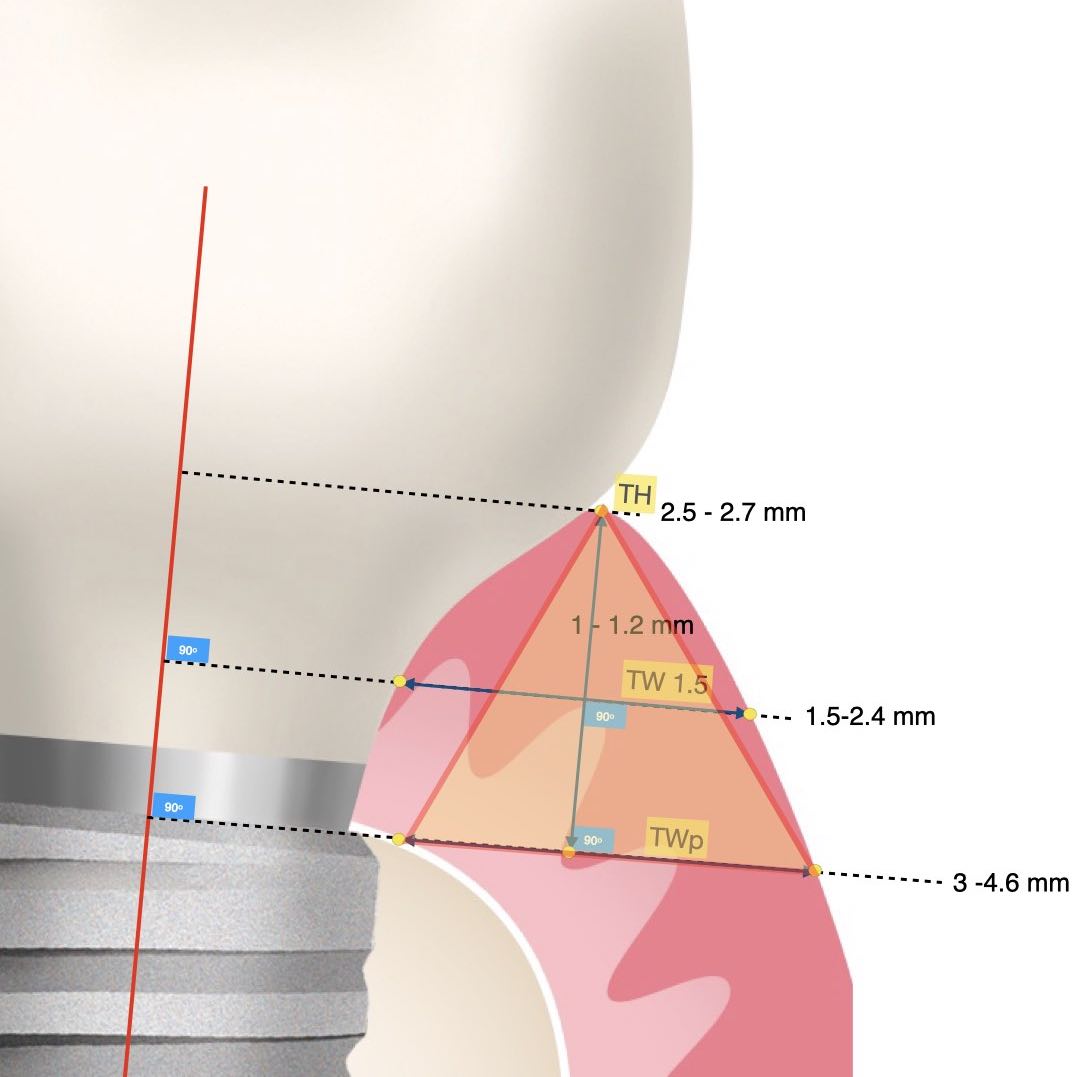
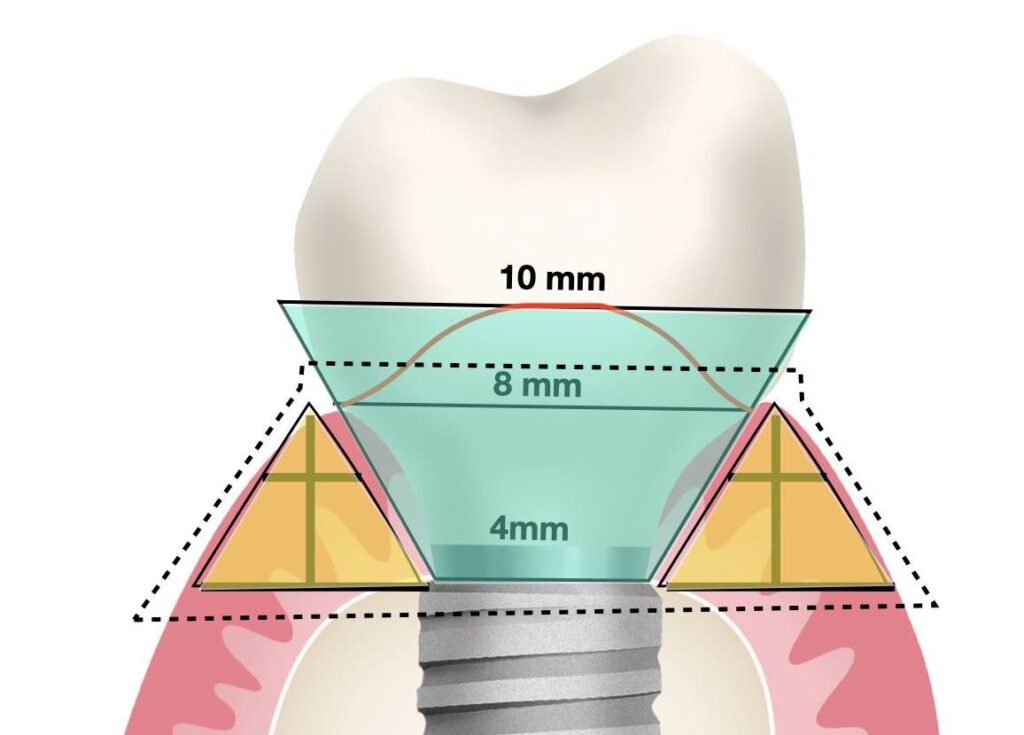
Through measurements of peri-implant mucosa, a consistent finding was always the mucosa being wider at its base than its height, resembling a pyramid.
A consistent finding in peri-implant mucosa dimensions was that the mucosal width at the implant platform was always more than the corresponding mucosa height. So in simple terms, if you draw a line at the level of osseointegration from the implant shoulder to the outside margin of the mucosa, this will always be more than the corresponding height of the soft tissue. In posterior sites the width will exceed the height by a factor of 1.5 to 2. Interestingly, this is the opposite in physiological periodontium, where the periodontal tissue around natural teeth are typically more high than wide. Now in the case of tissue level implants, the corresponding width is to be counted at the interface of the rough surface. Whether tissue or bone level implants, the vertical soft tissue architecture is being established on top of the marginal bone.
So thinking as an architect, the peri-implant mucosa resembles a Pyramid, where the wider the base the higher you can reach. On the contrary, the periodontal tissue looks more like a townhouse in Amsterdam: although really squeezed in width, it can still reach a 4-storey height! But for now it’s only nature that builds townhowses, we are into pyramids.
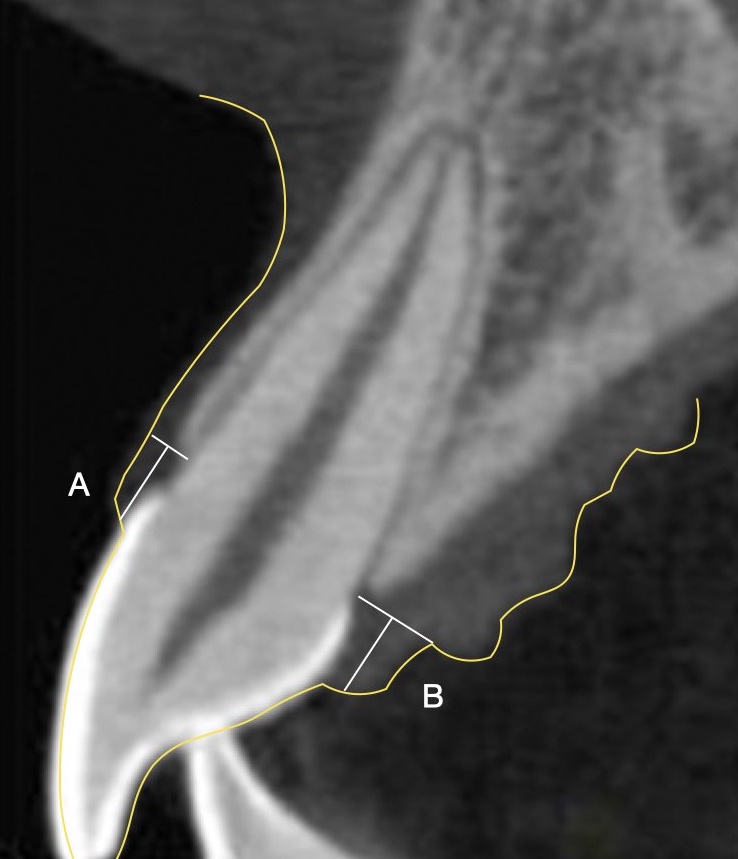
A townhowse of beautiful proportions:
Note the natural architecture of the periodontium, with a narrow base of the soft tissue at the margin of the bone and a longer dimension in height! This is especially pronounced at the buccal sites (A), but the base widens palatal (B) where the angle of the palatal alveolar ridge widens. Looks great, but don't try this with implants!
Periodontal vs Peri-implant "architecture"
Now the interesting thing is that both physiological periodontal and repair peri-implant mucosa appear to adhere to certain architectural fundamental rules, which in some aspects are very different. And here comes our part as the architects: violate the fundamental rules and the house will fall, no matter how fancy the technology.
A guide for meticulous architects:
So first thing to look for when trying to build the pyramid is a vast piece of flat land to set the base. Yes, we do need a certain minimum height of soft issue to establish a healthy and sustainable peri-implant tissue anatomy and the larger the flat base the higher you will be able to reach with your pyramid. But what is the best way to secure the flat land to build on?
When we discuss about tissue thickness, many will almost spontaneously jump to surgical solutions and soft tissue augmentation. Not so fast! Soft tissue augmentation has its place (and limitations), but in my hands its place is mainly in correcting deficiencies than a” pre-emptive” or “preventive” use. In anyway, before you consider soft tissue augmentation there are a couple of critical design parametres that do make a difference: implant position and prosthesis design!
As we discussed ,the pyramid will be build just next to our implant, thus the “flat land” we are looking for is primarily the circumferential bone around the implant. For example, considering that the most challenging aspect of the peri-implant mucosa dimensions in the aesthetic zone is typically in the buccal area, placing the implant in the palatal part of the prosthetic comfort zone can ensure more space for the “pyramid” base, even in the presence of thinner mucosa. This is also why a bone augmentation with GBR in the same location is in most cases enough to secure adequate soft tissue thickness as well, by establishing the essential base to support the pyramid. Sometimes the implant position might be slightly to the palatal side of the prosthetic comfort zone at the expense of the palatal tissue space, but in most cases the angle of the palatal bone results in supporting a wider pyramid of the palatal mucosa, with no impact in the aesthetics, which is thus less susceptible to problems.
A pyramid that holds!
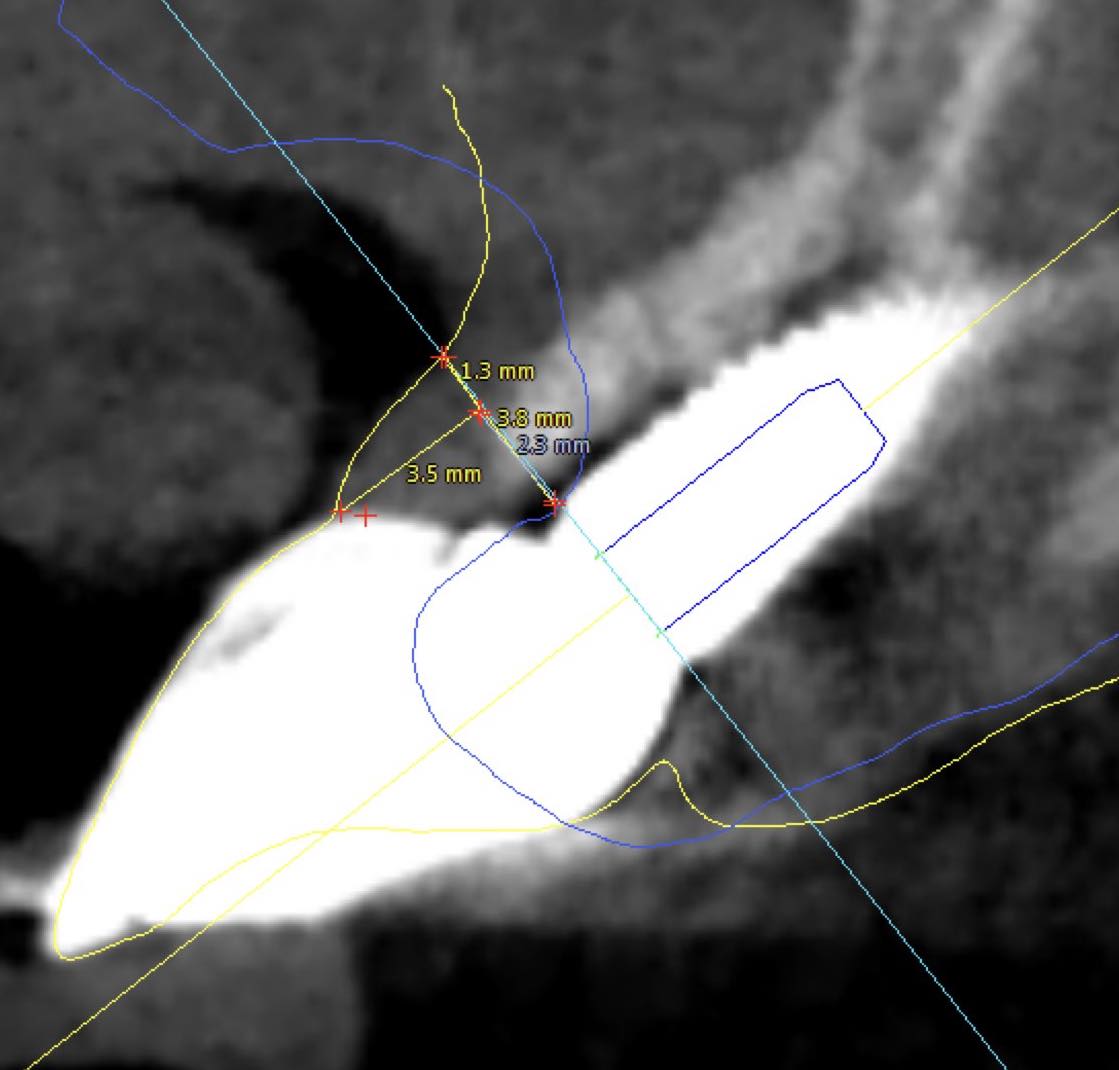
Observe the dimensions of the buccal peri-implant mucosa 18 months after implant placement with Guided Bone Regeneration of a self contained buccal bone defect. The overall mucosa before surgery was actually only 1.3 mm thick, but thanks to the augmentation of the bone, there is sufficient "flat land" to establish a wide base of the pyramid (5.1 mm) and the essential soft tissue height (3.5 mm).It's not a townhouse, it's a pyramid, but will do the job!
And last but not least, the design of the prosthesis of course: The Emergence Profile, the Transmucosal part of the abutment and the prosthesis. Remember, this is the reason that peri-implant tissue exists. This is the concrete wall we built next to the tree. That might explain how altering the shape of the Emergence profile from Concave to convex can predictably cause mucosal recession, an observation that we can use to our advantage or ignore to our detriment..! In essence, implant, prosthesis and mucosa are all parts of the same interrelated system, sharing the same space: enlarging one side, reduces the other!
A properly designed prosthesis matched with a proper implant position can go far into determining the shape and dimensions of the soft tissue. Don’t just place a crown – Engineer a system!
Of course there is an art and science behind all this and in reality in clinics there is also a art of compromise, that is select which feature you will introduce a compromise in if you have to, in order to secure the best balance in your outcomes between aesthetics, function and sustainable health.
But it’s Friday evening in Bangkok and the arriving weekend implies that it’s a good time to put a stop for now, leaving a more detailed discussion for next time! Enjoy your weekend and let’s build some great pyramids
6 thoughts on “peri-implant mucosa dimensions and emergence profile: a guide for meticulous architects”
Thank you for this article, very nice way to explain some complex ideas!
So what is the role of augmentations? is thicker tissue better for long term outcomes? Especially in case of immediat implants I hear a standard of using connective tissue. What is your thoughts?
Thnak you, very interesting thoughts and vivid description!
… Egypt, an endless source of inspiration 😁
beautiful article,thank you for sharing!
is this relates to the theory of the zones? I wonder if the critical-subcritical contours have similar implications
It is a great reminder that we do not recreate nature, just imitate it with poor and humble means. Save teeth, this is our mission!