Robotic implant surgery is already being hailed as the next frontier—a technological revolution promising unprecedented precision, improved outcomes, and even the holy grail of fully automated surgery. But let’s take a step back and ask: how far have we truly come? Will dental robotics ever become a mainstay rather than a niche curiosity? In this blog post we review the current state of the art in robotic Computer Assisted Implant Surgery and spot to find the next big thing in the near future!
Implant Dentistry Blog
Implant Dentistry is about creating a whole new organ. Balancing human tissues, mechanical components and bacteria, Dental Implants are the true Cyborgs of 21st century.
Computer Assisted Implant Surgery: A New Paradigm Unfolding!
The name might be misleading, because CAIS is not about computers, neither is it limited to surgery. CAIS is Implant Dentistry revisited, carefully re-orchstrated in a seamless workflow, which unlocks true and major benefits for your patients.
Click on the respective areas of the image below to see definitions and find related articles and content in this website!
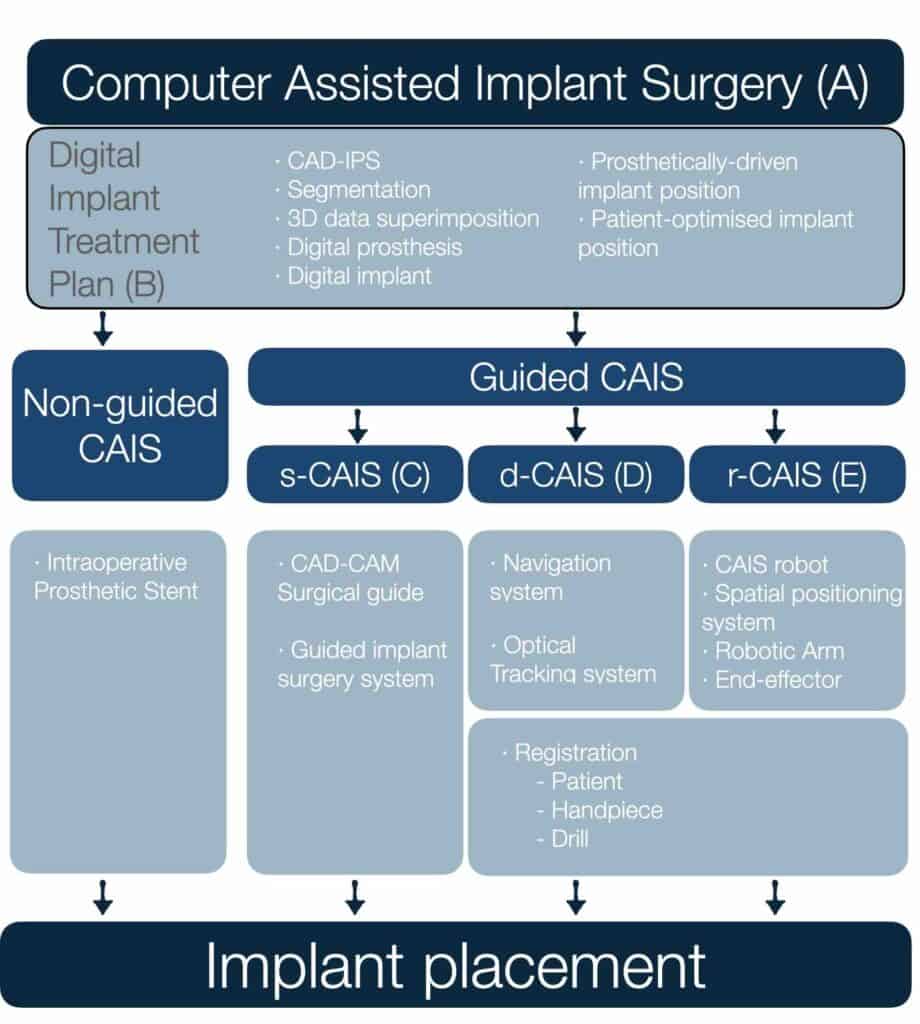
The use of digital technologies, software and devices to plan the patient-optimised 3D position of the dental implant, which will then be surgically placed by guided or non-guided means
→ Read more: P4 Implant Dentistry
The design of the virtual prosthesis, prosthetic components and implant type and position in appropriate relation to the patient's anatomic structures by means of digital technologies
→ Read more: Implant prosthesis design demystified
The use of robotic technology with varying levels of automation for planing and placement of dental implants under human supervision/control.
→Read more: Robotics in Implant Dentistry
The use of a navigation system to provide the surgeon with realtime spatial feedback during implant surgery.
→Read more: Is the future static or dynamic?
A system designed to provide real time guidance of surgical instruments used for osteotomies, implant site preparation and implant placement.
→Read more: Dynamic Navigation: understanding outcomes
The 3D implant position which fulfils all essential restorative, biological and surgical requirements.
→Read more: 1)Understanding the peri-implant mucosa architecture
2) Tissue or Bone Level?
The 3D implant position which is fully aligned with the design of the prosthesis and the supracrestal complex.
→Read more: The Implant Supracrestal Complex
The use of static, dynamic or robotic CAIS technologies for guiding implant surgery.
→Read more: CAIS in Clinical Practice
Master the use of dynamic navigation in immediacy in this unique 2-day masterclass in Bangkok!
→Visit now: 25-26 April in Bangkok
The use of CAD/CAM surgical guides technologies for guiding osteotomy, implant placement and related surgical procedures.
→Read more: Static, Dynamic or maybe both?
Computer-aided Designed and Manufactured (CAD/CAM) device aiming to guide the osteotomy and the placement of a dental implant in the planned position
→Read more: Static CAIS: where are we today?
Surgical preparation of an osteotomy and placement of the dental implant. Immediate, if placed in the fresh extraction socket.
→Read more: 1) Immediacy revisited! and 2) Immediacy in the Esthetic Zone
Primary stability at implant placement (attributed to friction), evolves through distant and contact osteogenesis into full osseointegration of the implant.
→Read more: From friction stability to Osseointegration
The use of Artificial Intelligence Algorithms for the virtual planing of implant treatment.
→Read more: Artificial Intelligence and Treatment Planing
Computer Assisted Design software specifically developed for the digital plan of dental implant treatment including the ability to perform detailed measurements.
→Read more: Artificial Intelligence and Treatment Planing
A spatial positioning system designed for real time spatial tracking of surgical instruments, position and orientation of the patient utilising optical technology and stereoscopic cameras.
→Read more: Key surgical skills with navigation
The process of "mapping" of an actual item dimensions and real-time position within a 3-dimensional coordinate system, such as the one created and maintained by the spatial positioning system of a navigation device.
→Read more: Key surgical skills with navigation
Read more:
Precision Medicine or P4 is a paradigm of care which considers a patient's individual characteristics to guide diagnosis and treatment. With the wide implementation of a digital workflow, implant dentistry is not fit for P4 practice focused on personalised care, preventive design, predictive algorithms and participatory engagement of the patient.
dental implants placed in fresh extraction sockets were first documented more than 25 years ago, so one might wonder why “immediacy” took so long time to mature into the mainstream implantology. The progress of a scientific protocol however, is rarely a straight line to implementation. Perceived breakthroughs are often followed by backlash and enthusiasm can be at times interchangeable with periods of caution. In the end, technology is also a major catalyst to help a vision make it safe to the mainstream practice.
How did immediacy develop from the first “immediate” implants into the current modern concept as a workflow? Let’s take a closer look into a long and winding road!
dental implants placed in fresh extraction sockets were first documented more than 25 years ago, so one might wonder why “immediacy” took so long time to mature into the mainstream implantology. The progress of a scientific protocol however, is rarely a straight line to implementation. Perceived breakthroughs are often followed by backlash and enthusiasm can be at times interchangeable with periods of caution. In the end, technology is also a major catalyst to help a vision make it safe to the mainstream practice.
How did immediacy develop from the first “immediate” implants into the current modern concept as a workflow? Let’s take a closer look into a long and winding road!
With Artificial Intelligence entering every aspect of healthcare, the already increasingly digitized field of Implant Dentistry has become a testing ground for new tools. But what is in the core of this “artificial intelligence” revolution and how different is it really to what we have been doing so far in Implantology? In this article we discuss fundamentals of what machine learning is and is not, we will discuss the concepts of intelligence and artificial intelligence and applications in healthcare and implantology and we will see how these models are susceptible to mistakes just like every other tools developed for diagnostics
Is the implant emergence profile important for success of treatment? A wide mucosal emergence angle of the implant prosthesis can increase by as much as 30 times the risk for inflammation of the peri-implant tissue, as shown by a recent clinical study. It becomes therefore apparent that the prosthetic design of the implant supracrestal complex is critical for the long-term health of peri-implant tissue. Read more about the design features that are most important and the designs you need to follow when treatment planning with dental implants. Mucosal Emergence Angle, Deep Angle, Total Contour Angle
Half a dozen major dynamic navigation systems focused in implant dentistry are now in the market, two of which are backed by leading implant manufacturers Straumann and Nobel Biocare. All systems use in principle the same optical tracking technology, but they each have its own proprietary design features which can impact ergonomics, accuracy, user experience, overall efficiency and cost effectiveness. The competition is going to be fierce and whether a clear winner is going to emerge in the end is up to everyone to speculate.
And while the masses will soon move into dynamic navigation, the early adopters are already documenting the rise of the robots! The marriage of the dynamic CAIS with the robotic arm has already borne fruit and the child is growing healthy and strong in two continents. Autonomous robotic implant systems are already in the market in US and China and although in an early stage of adoption, we see now the first peer-reviewed published results in the form of case series.
In a recent randomised clinical trial static and dynamic computer assisted implant surgery were combined and used simultaneously while placing dental implants. The result was increased accuracy, even beyond the level that static or dynamic CAIS alone can offer. This can lead to even more precise surgeries, It comes however with an increased cost and time commitment. How can you combine static and dynamic? Well that was not too difficult actually. In principle, you have to follow the workflow of the static, print the guide accordingly and then register and calibrate the guided surgery drills for the dynamic CAIS before the surgery. In the surgery the operator will place the surgical guide and continue with the drills as usual, only now with the visual aid of the correct angle and depth also displayed in real time.
Have you ever thought why some people are fast to orientate with a map, while others tend to be always lost? Or, why some prefer to look at the navigation carefully once before driving, while others need to have it constantly in front of their eyes? And what does this all have to do with implant surgery? Today we will dissect a crucial skill for any implant surgeon, the spatial representation ability and we will discuss how to train and improve it for the benefit of your patients. Finally we have a small challenge to test your skills!
In our first article 2 years ago we explored the difference between tissue level and bone level implants with regards to risk for peri-implantitis. In this article, we discuss deeper about the emergence profile in the light of new knowledge and we also extend to assess technical complications and potential implications of the implant connection. We will discusss the ocncept of Emergence profile and the "deep" emergence angle and we will investigate closer what were the reasons behind the early success of Tissue level implants, as well as their limitations.
Static and Dynamic computer assisted implant surgery appear to deliver the same level of accuracy if we study the average deviation. But this is only half the truth. By analysing frequencies instead of the mean we could see some important differences and clinical implications, as it becomes obvious that both dynamic and static CAIS will deliver "plug and play" immediacy in 40% of the cases, as opposed to only 10% for freehand. If we extend to include the small modification group then we see CAIS serving successfully as much as 80% of the cases! Think of the time and resources saved, the logistics and the patient experience and you have already a major benefit of CAIS, certainly not described in the previously reported means. That is of course if you follow an immediacy procedure. With a conventional loading protocol, the benefit of CAIS is probably not that important in clinical terms.
Computer Assisted Implant Surgery is increasingly popular, with almost every implant system racing to deliver the most reliable technology and protocols. Either as static or dynamic, CAIS promises unprecedented accuracy in implant placement and evidence now shows that it delivers. But is it just about accuracy? How reliable is this technology and how important is a millimetre after all? Is it worth the cost and trouble? Can this technology transform the way we practice implant dentistry, or will it remain a premium gadget mainly targeting complex cases in ‘up-market’ clinics?
These were some of our genuine questions when we embarked in a long project assessing computer assisted surgical technology in practice. If you share these questions, then the article that follows is for you!
Mechanical disinfection remains the cornerstone of the management of Peri-implantitis. But do we best achieve our goals? From simply rinsing with saline and rubbing with a gauze to a whole Er:Yag Lazer, there is a whole spectrum of techniques and devices that seem to achieve comparable results. How do we choose and where do we strike the best balance?
Read below for some clinical “tips and tricks” to help you make the most of each approach! In this article, we discuss plastic, carbon fibre and titanium curettes, ultrasonic and piezoelectric tips, titanium brushes and Labrida brush.
The use of soft tissue augmentation techniques to increase the keratinised with around dental implants has been debated since long. This article disusses the need of soft tissue augmentations, the main determinants for decision making and presents a minimally invasive grafting technique, the Hybrid CT-Epithelial graft.
Tissue level vs Bone level implants is a discussion that goes back to the very DNA of implant dentistry. The original implant designed by Branemark was a bone level implant, intended to be submerged fully under the bone. Then the Tissue level design was proposed by Schroeder and IT, where the implant included a transmucosal colar. In this article, we investigate the wide spread belief that the use of Tissue Level implants reduces the risk for peri-implantitis. Fact or Myth?
All journeys in implant dentistry start with aquiring “primary” stability, which is nothing but static friction between the newly placed implant and the bone. But nothing good ...
Back in the army we had an old ambulance which we called “Florence Nightingale”, in an obvious reference to its years in service. We used it to deliver medication and supplies ...
Peri-implantitis starts at the prosthesis of the dental implant, where the biofilm first accummulates. Understanding the interelation of the prosthesis with the complex system of tissue and bacteria is the key to prevent and mange peri-implant tissue inflammation, in the new paradigm of the The Implant Supracrestal Complex. This is a unifying concept in Implant Dentistry, where human tissue, mechanical components (implant, abutment, prosthesis) and bacteria are studied as one system. This way we can better understand the complex interactions that take place to determine health and disease and we can design more effective interventions to prevent and manage long term complications.
The Implant Supracrestal Complex is a unifying concept in Implant Dentistry, where human tissue, mechanical components (implant, abutment, prosthesis) and bacteria are studied as one system. This way we can better understand the complex interactions that take place to determine health and disease and we can design more effective interventions to prevent and manage long term complications.
In our previous post, we reviewed the older perceptions of the “Biologic Width” and concluded that there are two main zones of soft tissue around healthy implants: one genetically ...
From the very start of my training in Periodontology, I learned to see my probe as an Ultimate Judge. Three interchangeable lines – the magical reading of “3mm” – could split the ...
Immediate implants in the aesthetic zone remain a hotly debated topic with many enthusiasts among clinicians, as well as many sceptics.
This article aims to review current ...