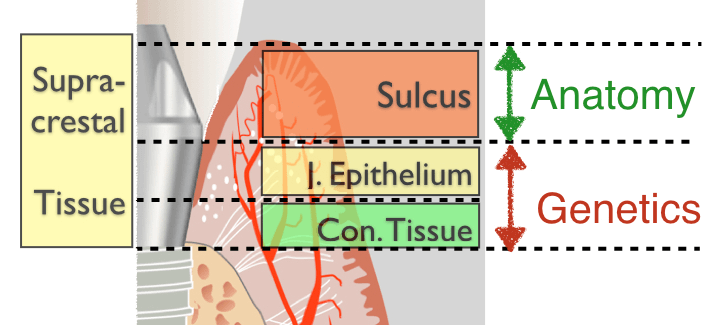
In our previous post, we reviewed the older perceptions of the “Biologic Width” and concluded that there are two main zones of soft tissue around healthy implants: one genetically determined that includes the junctional epithelium and the connective tissue and another, the peri-implant sulcus, which is influenced by many factors.
In this post, we will move from the animal to the human studies and compare the “Biologic Width” to the “Supracrestal Tissue”. We will then attempt to investigate how the peri-implant soft tissues form, in particular in the aesthetic zone!
The Biological Imperative
The early histological studies of the peri-implant tissues pointed out a biological imperative: Bone will be separated from the oral environment by three layers of soft tissue: the connective tissue, the junctional epithelium and the sulcus. In correspondence to teeth, these three layers were loosely named “Biologic Width”, and this was easy to perceive when implant dentistry was mainly limited to edentulous patients and full arch restorations.
However, the rise of the prosthetic-driven implant placement, in particular for single tooth replacement in the aesthetic zone called for a much more precise understanding of the soft tissue architecture around implants. So for the rest of this paper let us not use the term Biologic Width any more. Instead, we can talk of the supracrestal soft tissue, which is composed of the vertical sequence of the Connective Tissue zone (CT, adhesion), the Junctional Epithelium (JE, attachment) and the sulcus (S, free).
So what happens in humans?
A series of histological studies in humans were designed in the University of Gothenburg, using a custom made healing abutment, which was after the healing retrieved with a 1,5 mm thick layer of attached soft tissues. Tomasi et al. (1) studying human histology from implants in the premolar and molar region confirmed the structures we expected: at 12 weeks they found healed peri-implant soft tissues with an average of 2.4 mm vertical height, 1.6 mm of this was the epithelial component (J. Epithelium + Sulcus) and 0.8 mm the connective tissue zone. Two interesting points here: First, as the healing abutments were concave, the histology showed a horizontal offset of the soft tissues as well. Although the vertical height was 2.4 mm, the corresponding contact area facing the healing abutment was 3.2 mm.
Two interesting points here: First, as the healing abutments were concave, the histology showed a horizontal offset of the soft tissues as well. Although the vertical height was 2.4 mm, the corresponding contact area facing the healing abutment was 3.2 mm.
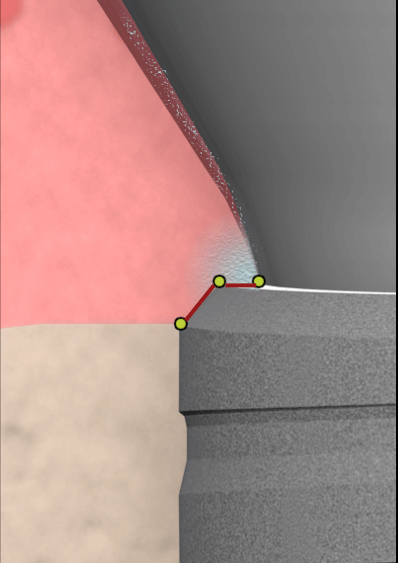
This is important, as most modern bone level implants come with “platform switching”, a concept that also allows for some horizontal offset of the Supracrestal tissues.
Some final numbers?
It also showed some significant variation between different people. Nevertheless, today there is an established understanding that a supracrestal tissue zone of about 3-4mm is a biological imperative (2). Allow for this zone to establish undisturbed and let nature care for the rest.
A Supracrestal soft tissue zone of about 3 mm in vertical dimension is a biological imperative
So, 3 mm should be enough?
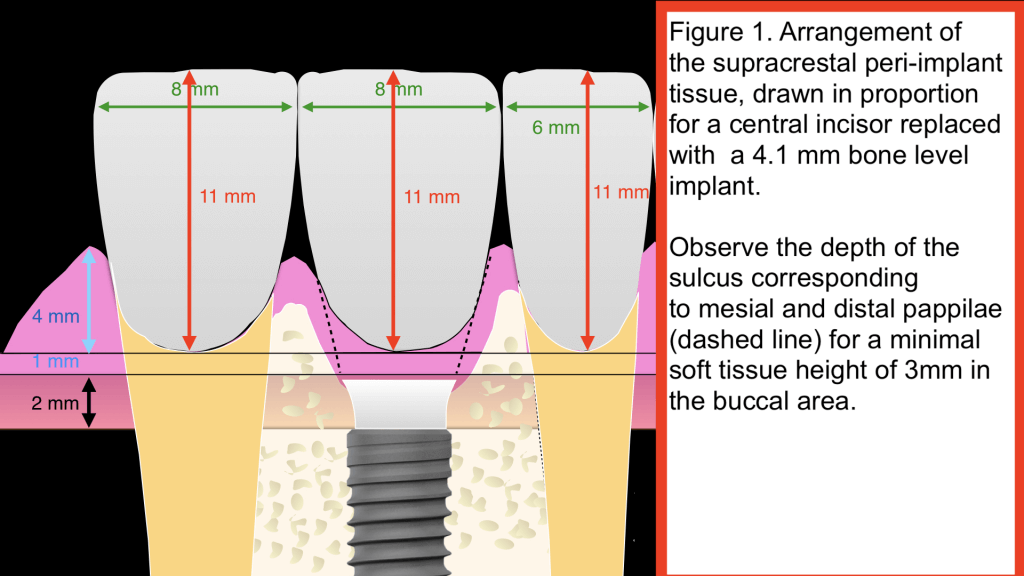
Well, yes, if you don’t mind a “flat” emergence profile, as we had in the older full arch prostheses or we would often still have in the posterior segments. In particular in the anterior maxilla however, the need for a natural and aesthetic emergence profile means that we need much higher supracrestal tissues mesial and distal to form papillae. Figure 1 is drawn in proportion, representing a typical central incisor.
To secure an aesthetic result in such a case would require an additional height of 3-5 mm at the papillae, on top of the minimum supracrestal tissue height of 3mm in the buccal area. Knowing that nobody has managed as of today to predictably manipulate the length of the Junctional Epithelium or the Connective Tissue, leaves us with only one outcome: Aesthetic implant placement results inevitably in a deep sulcus at the papillae area, a sulcus that can reach 4,5 or even 6 mm till the Junctional Epithelium.
Can we prevent the deep sulcus in the aesthetic zone?
Not, if we want to have a natural emergence profile and aesthetic outcomes. In the past, scalloped implants were developed and marketed in anticipation of better peri-implant tissue preservation. Unfortunately, scalloped implants brought more problems than they could resolve and were quickly discontinued.
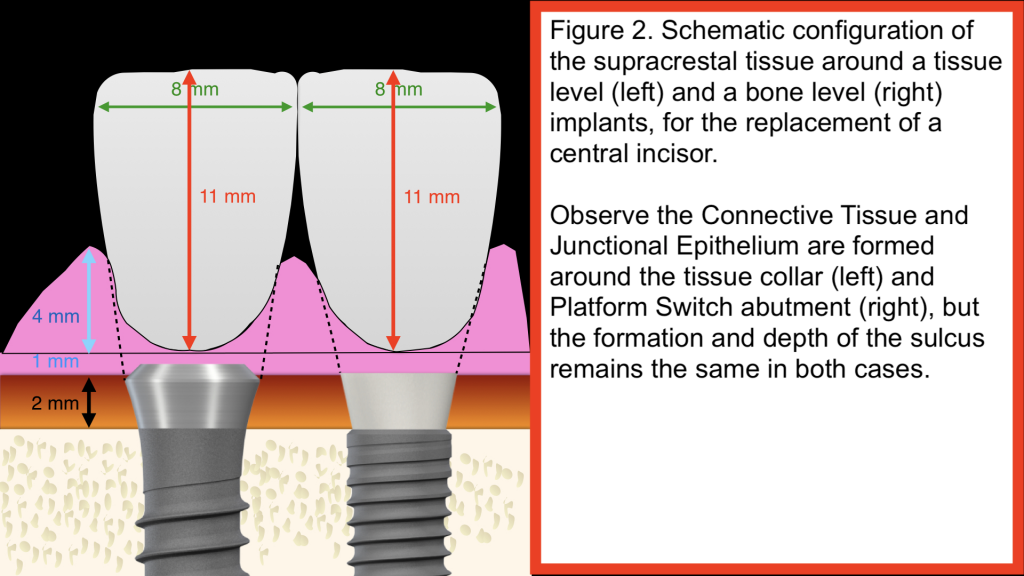
And what about tissue level implants?
Tissue level implants are my favourite implants in posterior sites, they will not, however, affect the depth of the sulcus. When placed in the aesthetic zone the supracrestal tissue outcomes of tissue level implants are no different to that of the bone level ones, because the prosthesis drives the placement. In Figure 2, we compare schematically a tissue and a bone level implant, placed for the replacement of a central incisor. The only difference is that the Tissue Level implant will establish the first 1.8mm of the supracrestal tissues (CT +JE) on its smooth collar, instead of the platform switching abutment, as will be the case in the bone level. The sulcus depth however on top will remain unchanged for both.
Having used tissue level implants in the anterior for many years in the past, I am convinced that they offer no advantage to Bone Level implants in the aesthetic zone, on the contrary, they allow little “buffer” when it comes to the ideal positioning and might come with certain risks. But maybe we can wait till the next post for a more detailed discussion about Tissue and Bone level implants in the anterior. Summing up, we have to conclude that at the current state of the art, aesthetic implant placement inevitably comes with a deep sulcus. Is this a “recipe for disaster”, an inherent limitation we need to acknowledge or a risk that we can account for and manage through our planning?
For this, let us discuss in more detail next time!
Coming Next:
The deep Sulcus: acceptable reality or a ticking bomb?– The Supracrestal Complex and how to keep it healthy in the long term?



4 thoughts on “Who’s afraid of the deep bad Sulcus…? (part 2)”
Great post
Thank you for your kind feedback!
Good article !
BTW if you can quote some reference, it’s much better !!
Thanks !
Greetings Dr.Mattheos,
I fully enjoyed the University of Hong Kong Coursera.
I come from a lab and clinical background. I noticed an emergence of different kinds of tissue level implants. Some tissue level implants are more sub-gingival while others are equigingival(ie: IBS Magicore dental implants). For the equigingival implants, I feel this makes the restoration impossible for the lab to design a crown which can impinge on the biologic width. What do you think?
Joseph Elizaga DMD